What to do if there is a white sore under your lip. What to do if you bite your cheek, tongue or lip and what the consequences may be
- chemical, thermal or mechanical damage to the lip;
- exposure to weather conditions in the form of wind, rain, cold, sun, etc.;
- viral infection;
- birth defects;
- oncology and others.
How to get rid of ulcers on the lips?
Often the appearance of various rashes and ulcers on the body is a consequence of slagging in the body, therefore effective way elimination - cleaning. As a result pathogenic bacteria, waste and toxins are easily removed naturally, which has a positive effect on the condition of the skin and mucous membranes.When the body becomes infected, a boil forms on the lip. At first it resembles a small reddish nodule, which quickly increases in size and is filled with purulent contents. The person also begins to experience general weakness, his body temperature rises, itching and burning appear. Treatment consists of using agents that accelerate the maturation of the abscess. Under no circumstances should you open it yourself; trust an experienced specialist. A prerequisite is to remove the pus completely to avoid relapse. After removing the purulent contents, it is necessary to monitor lip hygiene. To this end, injury that occurs during talking and eating solid food should be avoided.
If ulcers appear in the mouth, it is recommended to rinse with a solution of baking soda, table salt, or a decoction of calendula or chamomile. Efficiency lies in reducing painful sensations and relieving inflammation. Decoctions medicinal herbs have an anti-inflammatory effect.
Particularly dangerous are numerous rashes in the mouth area. It is better not to delay treatment. If the cause is damage to the body by the herpes virus, then it is regularly applied to the ulcers. antiviral drugs(“Acyclovir”, “Zovirax” and others), which destroy harmful microorganisms and accelerate the healing process.
Do not touch the affected area of the body with your hands, as the infection can spread throughout the body, which can lead to negative consequences.
During the treatment period, reconsider your diet, as a good immune system independently fights the causes of purulent rashes on the lips. It is advisable to enrich dishes with products with high content microelements and vitamins.
Pustular skin lesions - pyoderma - a group of acute and chronic diseases skin, which are caused by staphylococci, streptococci, and less commonly by other microorganisms. Provoke education ulcers insect bites, diaper rash, scratching and other microtraumas of the skin. Some forms of diseases in this group may be caused by disorders nervous system, diabetes mellitus and other metabolic diseases.
You will need
- - garlic;
- - alcohol 40%;
- - viburnum berries;
- - spruce resin;
- - wax;
- - butter;
- - burdock root;
- - elecampane root;
- - leaves walnut;
- - Echinacea purpurea root.
Instructions
Take equal amounts of mashed garlic and 40% alcohol, mix thoroughly, apply a layer on the affected area of the skin. Cover with compression paper and secure with a bandage. Change the mixture every 6 hours until complete recovery.
Mash 50 grams of viburnum berries and, placing them in a jar, pour 100 ml of 40% alcohol. After leaving for 2-3 days, lubricate the ulcers with the prepared composition, and at night, wet a cotton swab and secure it with a fixing bandage on the inflamed skin.
To remove an abscess, prepare a healing ointment based on spruce resin. Take equal amounts of spruce resin, natural wax, and butter. Place all ingredients in a saucepan and place it on water bath. Stirring constantly, heat until all ingredients are completely dissolved. Then strain through a layer of gauze and pour into a jar, which you store
The skin and mucous membrane of the lips are the thinnest and most vulnerable of all body tissues. Therefore, any pathological process easily affects this area. Lips perform a large number of functions, which explains the complexity of their structure. In addition to the fact that the lips delimit the initial part digestive tract, participate in the formation of the facial frame, form facial expressions, they also participate in the act of articulation. Located around the mouth opening huge amount muscles, both large - the orbicularis oris muscle, and small - many facial muscles. The lip is divided into 3 parts: the outer, inner and red border of the lips. The red border is a kind of transitional border. Most often, the pathology is localized here due to the fact that the skin in this area is very thin, and underneath there are a large number of blood vessels (hence the name).
Ulcer on the lip: causes
If you find that your lower lip hurts on the outside or inside, then you can suspect the following reasons that could cause the sore - an ulcer:
- the formation of microcracks as a result of tissue damage and subsequent contamination of the wound with microbial agents with the development of immune and inflammatory reactions;
- persistence of the herpes virus, which has become active due to decreased immunity, for example, as a result of hypothermia, acute respiratory viral infection or the common cold;
- burn;
- allergic reactions;
- manifestation of galvanism - when there are 2 dentures or any metal structures in the mouth, which, in contact with each other, generate an electric current, due to which a sore is formed;
- blockage of the excretory ducts of the salivary glands.
Pathogenesis of ulcer formation
Such an abundance of blood vessels causes the presence of a large number of immunocompetent cells and biologically active substances– inflammatory mediators that react acutely to pathogen penetration. And pathogens often penetrate the lip. Since the skin is vulnerable, and the lip is a part of the face that is constantly exposed to irritants, be it mechanical irritants in the form of rough food or temperature factors, they are very often susceptible to the formation of microcracks and pores. Microorganisms penetrate into these microcracks either from the external environment or from the oral cavity. That is, these cracks are the entrance gates pathological process. As a result of foreign invasion, the body's defense reactions are activated. The blood vessels of the lips narrow sharply, and then expand just as quickly. As a result, there is an abundant flow of blood and with it the body’s cells - leukocytes, monocytes, macrophages, neutrophils and others. They consume bacterial cells and die themselves. This lysis process releases microsomal enzymes that are capable of breaking down tissue. Similar reactions occur in absolutely any tissue if an invasion of a microorganism has occurred. However, in no other tissue except the lips does the formation of pathology occur - an ulcer, it would seem, due to such a trivial reason. And this happens due to the aforementioned thinness of the surface, the tissues melt faster under the action of enzymes, and a defect is formed - a painful ulcer on the lip from the inside.
In addition to microbial invasion, another common cause of ulcer formation on the inner surface of the lip is a disease such as herpes. Herpes is a virus. It affects humans most often in childhood or adolescence. In this case, a person suffers from an influenza-type disease, without even suspecting that the causative agent was herpes. After a single infection enters the body, it persists throughout life and cannot be eliminated. The herpes virus is usually localized in the peripheral nerve ganglia. In the normal state of the body, it is latent. However, as soon as any bad situation occurs that will lead to a weakening of the immune system, herpes will immediately make itself felt, and, basically, it manifests itself only on the mucous membrane of the lips.
![]()
Eating food that is too hot or getting anything caustic on your lips chemical compound can also cause the formation of ulcers on the inner surface of the lip.
Very often, an ulcer on the inside of the lower lip is formed as a result of immune desensitization. The skin of the lips is the first to come into contact with any allergens entering the oral cavity, so very often small vesicles, blisters and even ulcers can form on the surface, caused by the formation of immune complexes - antigen-antibody, which are deposited on the surface of the mucous membrane, causing the separation of this area from healthy tissue , thereby preventing generalization.
Diagnosis and treatment
If you find that you have pain in your lower or upper lip from the inside, then do not rush to panic. As already mentioned, the reason for such formation may be completely trivial. As a therapy, it is recommended to avoid eating rough, too hot foods or sour fruits, which will further irritate the surface, causing the process to worsen. If you are sure that the reason why the ulcer appeared on the inside of the lip is herpes, then you can use antiviral drugs. The most common such drugs are acyclovir and Zovirax. They can be in the form of ointments, as well as in the form of tablets for oral administration. Also, for faster and better healing of the process, you can use ointments levomekol, de-panthenol, metrogil, and antiseptic solutions. They are aimed at eliminating pathogens from the wound and increasing the rate of repair. If a white sore on the lip does not heal for a long time or often recurs, then it is necessary to consult a dentist, who will determine the cause of its appearance and suggest measures that will eliminate their appearance forever.
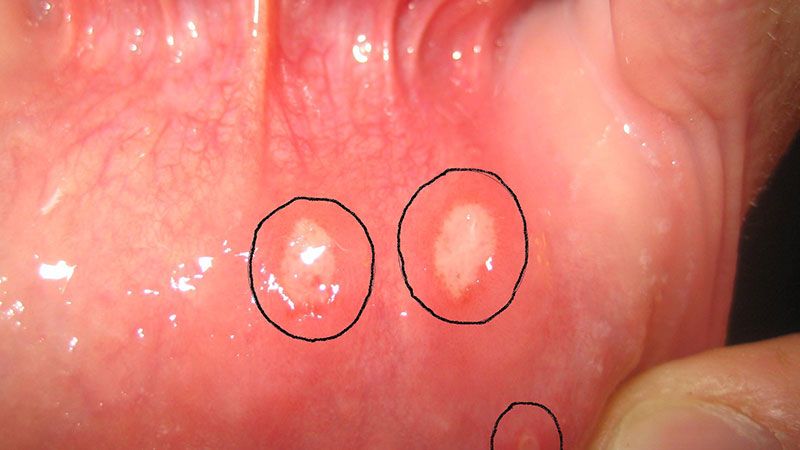
Aftoz Almost every fifth inhabitant of our planet suffers. Mouth ulcers represent a violation of the integrity of the mucous membrane of the gums, lips or cheeks. They can be grayish, white, red or yellowish in color. They often significantly worsen the quality of life, making it difficult to get food and even talk normally.
Reasons for appearance
The causes of ulcers in the mouth can be either specific diseases of the oral mucosa or general diseases of the body.Aphthous stomatitis in return form. This is inflammation that occurs in a chronic form. From time to time, aphthae rashes appear on the oral mucosa, which are quite painful. If aphthae has formed in a place of constant friction, then after its healing a scar may remain. In these patients, inflammation of the intestine is usually present. Often stomatitis develops against an emotional background, during menstruation. The aphthae scars within a week, but sometimes the process can take up to a month.
Stomatitis herpetiformis. With this disease, the lower plane of the tongue and the floor of the mouth are covered with small papules, reminiscent of herpetic rashes. The ulcers are not clearly defined; they are grayish in color. It takes about a week to a week and a half to heal.
Simple stomatitis characterized by the appearance of a white ulcer. In babies, white ulcers appear under the influence of candida or fungi.
Recurrent form of necrotizing periadenitis. The area of the mucous membrane thickens, after which an ulcer forms on it. Its surface is above the mucous membrane, it is painful and covered with infiltrate. This type of ulcer usually forms on the inner surfaces of the lips, the sides of the tongue, and the inner surfaces of the cheeks. The ulcers are so painful that many patients do not even eat during flare-ups. It's quite painful to talk. The disease occurs in a chronic form, and exacerbation can last for several months.
Afty Bednar. Only small patients who do not comply with hygienic requirements for oral care, as well as those who have a constant source of mechanical damage to the mucous membrane, are predisposed to this disease. The ulcers are yellowish in color and are located on the mucous membrane of the palate.
Traumatic mouth ulcers appear after injury. Most often, the injury occurs during teeth cleaning or dental treatment. An incorrectly fitted denture can cause ulcers. The ulcer heals in one and a half to two weeks if the mechanical impact is stopped. Usually no special therapy is even required. This type of ulcer does not hurt at all and is small.
Tuberculosis of the oral mucosa develops against the background of the lungs when the pathogen penetrates the oral mucosa. The first sign is small mounds, in place of which a little later ulcers form, gradually growing. The ulcer is small, its bottom is formed by bleeding epithelial cells. The pain is acute. The patient loses weight, the tongue is coated, the work of the sweat glands increases, and the body temperature increases.
Syphilis. At the end of the incubation period, ulcers appear on the oral mucosa, which do not completely go away until the final cure. They are round or ellipsoidal in shape, not painful, scarlet in color, with a glossy surface. After their scarring, star-shaped scars remain. Each ulcer lasts from 3 to 12 weeks. The mucous membrane around the ulcer is swollen, bluish in color and rises above the general level.
Gingivostomatitis in acute necrotic form it is provoked by a virus. Typically, ulcers cover the cheeks, gums, soft palate, and tonsils. Develops against the background of a fall, injury, hypothermia,. In some cases, the cause of the disease is. In patients ( men get sick more often), bad breath, acute pain while eating, increased production of saliva, increased body temperature. The mucous membrane swells, and when touched, blood flows from it.
In a child
 In children, mouth ulcers most often develop due to stomatitis. White or red spots appear on the mucous membrane of the mouth, the tongue swells, and the spots itch.
In children, mouth ulcers most often develop due to stomatitis. White or red spots appear on the mucous membrane of the mouth, the tongue swells, and the spots itch. Most often, this disease is not at all dangerous, but it worsens the child’s condition; he becomes capricious and eats poorly.
Stomatitis most often develops in weakened children prone to allergies. Sometimes it can indicate the presence of quite serious illnesses.
You should immediately take your child to the pediatrician if:
- Ulcers in the mouth are combined with blisters on the body,
- The child's body temperature has risen to 39 degrees or higher,
- Inflamed mucous membranes of the eyes or genitals,
- The ulcers appeared after the baby began treatment with any drug,
- The child complains of itching, it is difficult for him to breathe,
- If the ulcer is more than a centimeter across or there are a lot of them,
- If new ones appear before the old ones are scarred,
- Ulcers appear quite often,
- They do not scar for longer than 20 days.
Herpetic stomatitis usually affects children between one and three years of age. The mucous membrane of the mouth becomes covered with a large number of small papules, which rupture and ulcers remain in their place. There are sometimes about 100 papules. Body temperature may increase, regional swelling may swell and become painful. lymph nodes. This is a highly contagious disease that usually goes away within a couple of weeks.
Candidal stomatitis usually affects babies under one year of age. On the child's mucous membrane, areas covered with a dense coating appear, which are very itchy and very disturbing to the child. If you pick off the plaque, you will find bleeding tissue underneath. The baby does not want to eat, sleeps poorly, and is especially capricious while eating.
Allergic stomatitis develops under the influence of any allergens. These could be:
- Ingredients of toothpastes
- Medicines for treating the oral cavity,
- Substances used by dentists in treating children's teeth.
For HIV
Ulcers and other painful phenomena in the mouth are observed on average in 50% of infected people. Most often these are lesions that develop under the influence of candida. Atypical ulcers may also develop. Yeast-like candida fungi cause angular cheilitis, erythematous candidiasis and pseudomembranous candidiasis.Next, you can get acquainted with the most common conditions in people infected with HIV that occur with the formation of ulcers in the mouth.
Angular cheilitis This is the appearance of ulcers and cracks in the corners of the mouth. Often ulcers are combined with other manifestations of candidiasis. If you do not undergo special therapy, the disease can last for years.
Erythematous candidiasis– are scarlet flat ulcers in the oral cavity. Most often the hard palate or tongue is affected. The patient suffers from a burning sensation while eating.
Pseudomembranous candidiasis- this is the formation of white spots resembling pieces of cottage cheese. They can be removed, then a wound will form under them.
Infections with another pathogen, histoplasma, can cause death in every fourth case, since histoplasma affects the entire body. Large ulcers and bumps appear on the mucous membranes of the patient’s mouth, and the edges of the ulcers are covered with overgrown tissue.
Necrotizing periodontitis and gingivitis manifested by the fact that with gingivitis, ulcers form on soft tissues, with periodontitis, periodontal tissue is affected. This disease indicates complete absence immunity. The patient experiences acute pain, his breath smells very bad, his teeth fall out, and large ulcers appear on his gums. In this case, the pain is felt as if it hurts somewhere deep in the jaw.
Herpes simplex virus causes large ulcers formed by a collection of small papules with cloudy fluid inside. Gingivostomatitis also develops under the influence of the same virus. The patient develops papules on the mucous membranes, which soon burst. In their place, ulcers of a fairly large diameter are formed ( up to 3 centimeters). They scar within 14 days. HIV-infected people are characterized by very frequent recurrences of this disease.
Quite common aphthous ulcers. Medicine cannot yet answer why they appear. With HIV, such mouth ulcers cause a lot of suffering. The patient cannot eat spicy, sour, salty, tough or hard foods. In addition, with impaired immunity, ulcers do not go away for more than ten weeks.
Neutropenic ulcers cause a lot of suffering. They form on any part of the mucous membrane. They appear in those patients whose level of absolute granulocyte content is less than 800 per milliliter of blood. Recently, the number of HIV-infected people with such ulcers has been increasing.
Traumatic ulcer
If an ulcer in the mouth appears after physical impact, it is called traumatic. The cause of its appearance may be eating too hot food, injury to teeth, dentures, or a toothbrush. Thus, an ulcer appears at the site of a wound, scratch or. In rare cases, the injury is caused by the dentist and much more often by the patient himself. Ulcers that appear as a result of injury from a prosthesis are very common; they are called prosthetic ulcers. Such ulcers are formed when dentures that are too large are poorly fitted or when their surface is rough.They rarely rise above the surface of the mucous membrane, usually round or elliptical in shape. Their size almost never exceeds a centimeter. The middle of the ulcer is a pale scab, which is surrounded by a red border. Such an ulcer will heal within one and a half to two weeks, but only if the cause of its appearance is eliminated.
As a rule, they do not cause inconvenience, so they go away on their own without patient intervention. If the ulcers are large enough and also painful, treatment is carried out under local anesthesia.
Sometimes ulcers appear due to radiation, exposure chemicals as well as frostbite.
White – aphthous stomatitis
Aphthous stomatitis is an inflammation of the oral mucosa, in which erosions form on the surface layer. This is a very painful process, which sometimes occurs with an increase in body temperature. If the patient's defenses are weak, the disease may return, which is chronic.Despite the fact that the causes and mechanism of development of this disease have not yet been fully studied, it is known for sure that the use of toothpastes and mouth rinses with sodium lauryl sulfate creates favorable conditions for the development of the disease. This substance is introduced to increase foam, it dehydrates the mucous membrane, which is not physiological norm. Sometimes changing toothpaste leads to a complete cure.
Often the cause of aphthosis is trauma to the oral mucosa. Almost half of dental patients say that their cheek was bitten before the ulcer appeared. And against the background of emotional or physical stress, the body’s defenses decrease and ulcers appear. The vast majority of patients with aphthous stomatitis do not eat properly, their diet lacks any minerals. The lack of iron, selenium, zinc, folic acid, group vitamins IN or WITH .
Foods that cause mouth ulcers:
- Citrus,
- Wheat, barley, buckwheat, rye,
- Pineapples,
- Figs,
- seafood,
- Seasonings,
- Hard cheeses,
- Chocolate.
Red – erythroplakia
Such formations are completely painless. They appear as red spots on the mucous membrane of the mouth. They usually appear under the tongue in a fold of tissue, on the tongue. Very often they appear among lovers of chewing tobacco and alcohol. With this disease, the mucous membrane atrophies, so visible blood vessels. This is where the red color of the fabric comes from. Education has clear boundaries and most often affects people over 55 years of age.There are several varieties of this disease in which the red spot may be covered with white dots or patches. The presence of erythroplakia is a reason to visit a doctor and submit tissue for biopsy, since nine out of ten patients have tissue malignancy. Almost every fifth patient has more than one focus of the disease in the oral cavity.
If small white spots are visible against the general red surface, the cause of the disease may be the yeast-like fungus Candida. Therefore, it is necessary to carry out an analysis of the bacteriological composition. But a biopsy is also necessary in this case, because erythroplakia is a precancerous condition.
There are pockets in the corners of the mouth
The first reason that causes redness in the corners of the mouth, and subsequently the appearance of cracks and ulcers, is a lack of vitamin B2 . A person becomes lethargic, the wings of his nose may peel off, and his tongue may burn.Sometimes an incorrectly selected denture also leads to the formation of a jam. Babies who like to lick their lips may also suffer from sores in the corners of their mouth. If this unpleasant phenomenon occurs in an adult, you should pay attention to the composition of the toothpaste. The presence of fluoride sometimes leads to its development.
If vitamin therapy and changing oral care products do not help, tissue scrapings should be taken for pathogenic microflora.
Be sure to eliminate all sources of infection in the oral cavity.
Introduce chicken eggs, cheese, chicken meat, fish, beans and peas, spinach, sorrel, cabbage, and nuts into the diet.
If a fungus is detected, desserts should be excluded for the time being. Lips should be lubricated with vitamin oil preparation E
or vegetable oil.
Treatment
Treatment of ulcers caused by stomatitis should take place in several stages. The treatment regimen is influenced by the severity of the disease, as well as the frequency of relapses. Treatment of patients of any age is carried out according to the same scheme. Only age-appropriate dosages are selected.
Treatment may be most effective when started immediately after the ulcer forms.
1. Baking soda. It can be used to irrigate the oral cavity in the following proportion: 1 teaspoon of soda per 150 ml of water. Irrigation should be carried out every two hours. Once every 3 hours, the sore can be treated with soda, slightly diluted with water until it becomes sour cream. Brush your teeth with soda until the ulcers heal.
2. Change your toothbrush. You can also boil the old one in water and soda.
3. Treat ulcers with brilliant green. It's pretty effective remedy, which really causes pain, especially if the ulcer is large.
If all of the above does not help, you can try other methods:
1.
Treat ulcers with lidocaine gels.
2.
Treat ulcers with dexamethasone gel.
3.
Rinse your mouth with antiseptics from the pharmacy.
4.
Mix the contents of 2 vitamin ampoules B12
and one ampoule of dexamethasone, add 2 crushed nystatin tablets. Soak small cotton wool flagella in the medicine and apply them for 10 minutes three or four times a day. If relief does not occur, treatment should be repeated.
5.
When ulcers appear on the red border of the lips, the diagnosis can be confidently made.
"and use Acyclovir ointment.
6.
Take antihistamines orally ( loratadine, tavegil, suprastin) or desensitizers ( fenkarol).
It is also possible to use products designed directly for damage to the mucous membrane. To speed up the recovery process, it is necessary to protect the damage site. Aftofix is designed specifically to solve this problem. After application, the drug creates a protective film that is permanently attached to the mucous membrane and prevents further injury and irritation of the ulcer. But in addition to the protective function, Aftofix contains components that promote natural recovery. The drug can be used for burns of the mucous membrane, bites and other mechanical damage, as well as inflammation of the mucous membrane. You can learn more about the product from the video:
How to get rid of exacerbations?
Some forms of stomatitis return quite often. The impetus for the deterioration of the condition can be stress, a sore in the mouth, or fatigue.There are measures to make remissions longer:
- Eliminate all carious cavities in teeth,
- Brush your teeth with toothpaste twice a day and rinse your mouth after every meal. Spend at least 3 minutes brushing your teeth, choose a brush with soft bristles,
- Avoid antimicrobial rinses and mouth balms
- Completely avoid foods that cause allergies
- Read the list of foods that can cause ulcers and exclude them from the menu for 2–3 weeks.
- Drink vitamin and mineral complexes twice a year,
- Get enough rest. ointments that significantly reduce the duration of the disease.
Treatment with traditional methods
1. Mash three large cloves of garlic and combine with two teaspoons of natural yogurt or curdled milk. Coat the sore areas, put it in your mouth and hold. Do it several times.2. Shred raw potatoes, apply to the sore spot.
3. Squeeze juice from carrots and irrigate mouth fresh juice, mixed with water in equal parts.
4. Squeeze the juice from the cabbage and irrigate the mouth, mixing it with water in equal parts.
5. Infuse 50 gr. St. John's wort in 100 ml of alcohol or vodka for 7 days. Dilute the tincture in a proportion of 35 drops per 100 ml of water, rinse your mouth. Drink 50 drops.
6. 1 tbsp. Brew 200 ml of boiling water for flat-leaved eryngium plants, leave until cool, add 4 grams boric acid. Use to irrigate the oral cavity.
7. 1 tbsp. Potentilla roots pour 200 ml of water at room temperature overnight, boil. Use to irrigate the oral cavity.
8. Brew 20 grams of oak bark with 200 ml of boiling water and keep in a water bath for half an hour. Cool, add water to the original amount. Irrigate your mouth.
9. Brew a tablespoon of chopped walnut leaves with 200 ml of boiling water, hold for half an hour and pass through a sieve. Use to irrigate the mouth in the following proportion: one dessert spoon per 100 ml of water. The procedures are carried out three times a day for one and a half to two weeks.
10. 1 teaspoon of calendula alcohol infusion ( sold in a pharmacy) dilute with half a glass of water and use to irrigate the oral cavity.
Biting a cheek, lip or tongue usually occurs unexpectedly: sharp pain at the same time, it seems to paralyze a person, and the mood deteriorates for a long time.
It’s good if the bite was not strong, and after a couple of hours the sufferer has already forgotten about the incident. But sometimes a bite provokes a real disaster, which then takes a long time to heal. And regular and frequent bites of the oral mucosa or tongue can be a harbinger of a dangerous condition.
What do you need to know about “self-bites” in order to take the necessary measures in time?
There are many reasons for accidental bites. Hasty and careless people often bite themselves. An enthusiastic conversation with intense emotions, plus a quick lunch - and now the person has already bitten his tongue or lip. Those who like to snack during physical activity are also at risk.
The brain cannot simultaneously process two complex tasks, and while a person is focused on one, the second one fails. Cheeks are often bitten during active play or sports.
For an accidental bite to occur, it is not necessary to have an abnormal jaw structure or mental problems. But if there is one or the other, the risk of biting yourself increases significantly, even in a calm environment or during sleep.
People suffering from diarrhea may clench their jaws so tightly in their sleep that a loud grinding noise is heard. In this case, the mucous membrane of the cheek or tongue may become trapped between the teeth. In addition to a psychological reason, bruxism also has a dental one. Those who neglect treatment risk one day simply biting off a piece of their cheek or tongue.
Certain features of the dental and jaw structure can also cause persistent biting of the cheek, tongue or lip area:

Special mention should be made nervous people and persons with mental disorders. They can “gnaw” the mucous membranes of their mouth for a long time and not even notice it until medical intervention is needed.
First aid - help yourself
Not every bite injury requires urgent appeal V medical institution, especially on the first day. But any bite requires reinsurance - taking measures at home. Therefore, if a person bites his tongue, inner side cheeks or lip, regardless of whether a visit to the doctor is planned or not, he needs to follow a number of simple recommendations:

What is prohibited to do
Self-medication can make the problem worse. After biting your tongue or mucous membranes, you should absolutely not:
- apply iodine, brilliant green or hydrogen peroxide to the wound;
- use or drink herbal infusions hot;
- rub the wound with your finger (tongue);
- nibble the edges of the wound;
- put dirty hands into your mouth;
- apply crushed tablets (antibiotics) to the wound.
What are the consequences of “self-eating”?
If a “self-bite” happens occasionally, and after that the person follows all the rules, the wound in most cases heals successfully. But sometimes, due to a careless attitude towards oneself or due to some other factors, secondary conditions develop - dangerous to health and life.
"Language Wars"
 The best thing that can happen with a tongue injury is long-term pain.
The best thing that can happen with a tongue injury is long-term pain.
This fleshy organ takes a long and painful time to heal, especially if the person has bitten his tongue very hard and the wound is deep.
Other consequences of bite are associated with infection and represent a chain of conditions arising from each other:
- . A tongue subject to inflammation changes its color and structure. There is discomfort, a slight burning sensation, and the person may lose the sense of taste.
- Abscess. The tongue begins to swell from the inside, and the person cannot eat or speak normally due to pain.
- Phlegmon. The inflammation reaches the point that the patient is no longer able to swallow or even breathe normally. Such a person is indicated for urgent hospitalization.
Damage to the buccal mucosa
Soft tissues heal quickly, but at the same time a pathogenic agent may have time to get into the wound. Typically, injuries to the buccal mucosa accompanied by infection lead to the following complications:
- . The disease is prone to relapse. It is a collection of small ulcers on areas of the oral mucosa that cause unbearable pain to a person.
- . Herpes lives in the bloodstream of 99% of people, so with low immunity there is a high risk that this virus will “wake up” and colonize the wound. With such a lesion, crowded small bubbles with liquid inside settle on the mucous membrane around the injured area.
- Afta Bednara. The disease mainly affects children. A special type of bacteria begins to multiply in the wound due to poor hygiene oral cavity. The mucous membrane becomes covered with a yellowish coating.
Teeth on lips...
There is a lot of loose fiber in the lips and a strong bite can not only cause a wound, but cut off part of it. After biting your lip, the following complications may occur: 
- Hematoma. Internal bleeding after biting can be quite severe. The lip swells, becomes painful, and its functions are partially impaired. A hematoma may have complications such as purulent inflammation, which is very dangerous. The temperature rises to 40 degrees.
- Inflammation. When an infection gets into the wound, the lip swells and fills with purulent exudate. The patient feels an unpleasant odor emanating from the site of injury. The condition requires urgent treatment.
What to do if ulcers and wounds appear at the site of the bite?
If, as a result of a bite, a scattering of ulcers or other formations have formed on the mucous membrane of the cheeks, lips or tongue that cause pain and prevent you from eating normally, the first thing you need to do is consult a dentist, who will determine the nature of the complication and prescribe the correct treatment.
But what to do if a person bites his tongue or lip out of town or on the weekend and there is no opportunity to urgently visit a doctor? Then you can try to help yourself at home by performing the following procedures.
For language:
- to speed up the healing of ulcers, you can use regular brilliant green;
- dilute Furacilin in plain water in a 1:1 ratio and use as a mouth rinse;
- Apply hydrogen peroxide to the ulcers twice a day;
- traditional method: brew herbal tea from oak bark, chamomile, thyme, sage and St. John's wort - then cool and rinse your mouth, trying to hold the decoction longer on the tongue.
Providing assistance to the buccal mucosa: 
- at moderate pain ulcers can be cauterized with hydrogen peroxide or Furacilin - these drugs are freely sold in any pharmacy;
- at severe pain it is recommended to buy a suspension of glycerin and novocaine (5 or 10%) and treat painful points;
- to make ulcers heal faster, they are lubricated with Kalanchoe juice or corticosteroid ointments;
- traditional method: mash two cloves of garlic, add a spoonful of yogurt or curdled milk, mix and apply to painful areas for a few minutes.
If you bite your lip:
- lubricate the lesions with honey or soda solution;
- treat with brilliant green (but it is very painful);
- buy Acyclovir ointment and apply to ulcers located on the outside of the lip;
- apply tea bags to the affected areas;
5 reasons to see a doctor
It is good to have self-medication skills, but there are situations when life literally depends on the help of qualified specialists. These five reasons are an urgent reason to see a doctor:
- 4 days have passed, but the mucous membrane continues to hurt and bleed.
- after 2 days of self-medication, the wound began to increase in size.
- if a large blue hematoma has grown at the site of the bite.
- if part of the lip or tongue is bitten off.
- the wound is more than 5 mm in length.
You can contact either a dentist or an ENT doctor if there is at least one of the stated reasons.
Folk signs
 If you bite your cheek, tongue or lip, do not rush to panic or get upset; most likely, this is a sign of upcoming changes in your life.
If you bite your cheek, tongue or lip, do not rush to panic or get upset; most likely, this is a sign of upcoming changes in your life.
They say that biting your tongue during a long conversation means an imminent conflict. Therefore, it is worth slowing down the discussion before it leads to a quarrel. And a person who bites his lip is considered an ill-wisher and a talker. Isn't that you?
Biting your cheek means you will soon receive a passionate kiss. But if the bite happened during sleep, then your cherished dreams may not come true.
Whatever the reason for biting, you need to take remedial measures and be more careful with your teeth in the future.
