Undigested food in stool. Undigested food in a child's stool.
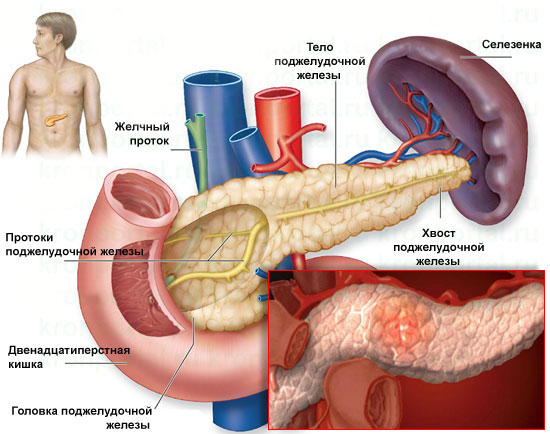
Pancreatitis is usually called a series of changes in the functioning of the pancreas associated with inflammation of its walls and disruption of important functional abilities. At the same time, its secretory function is disrupted, as a result of which the produced enzymes do not enter the duodenum, but remain in the pancreas itself, leading to deformation and changes in the structure of the mucous walls. It is customary to distinguish between acute and chronic pancreatitis. They differ from each other in their clinical manifestations.
Symptoms of pancreatitis in adults are observed among patients, most of whom abuse alcohol or have a history of gastrointestinal diseases. This condition is difficult to tolerate and requires urgent hospitalization, since the pancreas begins to “digest” its own walls, which can lead to very serious consequences. Patients with signs of acute pancreatitis are subject to hospitalization and treatment in a hospital.
Symptoms of acute pancreatitis are characterized by a violation of the outflow of pancreatic juice, as a result of which it enters the gland itself, causing severe pain. The pain is localized mainly in the left half of the abdomen, but after 20-30 minutes it becomes unbearable, widespread and covers the entire abdominal cavity.
Severe nausea, profuse vomiting, signs of intoxication appear - headache, muscle spasms, fever. Due to profuse and frequent vomiting, patients with acute pancreatitis feel very bad, become apathetic, weakened, and may lose consciousness.
The skin turns pale and sticky sweat begins to appear. In this condition, it often decreases blood pressure, memory and perception of surrounding objects are impaired. If urgent surgical care is not provided, a state of shock occurs.
Due to the rapid progression of acute pancreatitis, a large part of the pancreas dies, and internal organs located nearby may also be affected. If enzymes penetrate into the peritoneum, severe peritonitis of an aseptic type develops, directly threatening the patient’s life and capable of leading to death. Symptoms of pancreatitis in adults, in addition to pain, are characterized by symptoms of diarrhea with the presence of undigested food residues and traces of foam in the stool. The stool may have a foul odor.
Symptoms of chronic pancreatitis in adults
Chronic pancreatitis can occur without pronounced symptoms, masquerading as common illnesses gastrointestinal tract- gastritis, duodenal reflux, biliary dyskinesia.
Chronic inflammation of the pancreas can occur against the background of acute pancreatitis, cholelithiasis, alcoholism, poor nutrition and many years of overeating. In the initial period, which can last decades, patients mainly note constant pain in the abdomen, which radiates to the sternum, lower back and heart, misleading both the patients themselves and medical workers. A painful attack usually occurs some time after eating.
A relapse can be triggered by eating fried, smoked or excessively heavy foods, drinking cocoa-containing products, alcohol, marinades and carbonated drinks. Accompanied by exacerbation of dyspeptic disorders: nausea, vomiting, heartburn, stool disorders, gas formation. A painful attack can be easily relieved. The secretory function of the pancreas is not impaired at this stage. 
If chronic pancreatitis is observed in a patient for 10 years or more, then a new stage of the pathological process begins, in which serious changes occur in the structure of the mucous membrane of the pancreas with disruption of its secretory function.
The pain may disappear completely or be less noticeable. The pancreas ceases to fully synthesize hormones and enzymes necessary for normal digestion. Secretory insufficiency begins to develop, accompanied by impaired digestion of food (maldigestion) and a failure in the absorption of nutrients in the small intestine (malabsorption).
In this case, the patient complains of liquefaction of the stool and the presence of food fragments in it. The stool itself is quite copious, often with an unpleasant, fetid odor and increased fat content. This condition is quite dangerous for the patient, since with it most of the vitamins and microelements are simply not absorbed by the body, provoking the development of vitamin deficiency.
During fasting, pain usually calms down; therefore, many patients with chronic pancreatitis eat little and rapidly lose weight. It has been noticed that painful attacks rarely occur before lunch and occur in the late afternoon, intensifying when the patient bends the body forward.
A person with long-term chronic pancreatitis notes all the symptoms of vitamin deficiency and pancreatic dysfunction:
- blurred vision;
- weakened immunity;
- hair loss;
- dry skin and mucous membranes;
- bleeding gums;
- neuropsychiatric disorders;
- weakness, low blood pressure;
- dizziness, loss of consciousness;
- signs of osteoporosis;
- the occurrence of cramps in the calf muscles, thighs;
- thirst, low blood sugar.
Most patients with chronic pancreatitis suffer from a carbohydrate metabolism disorder. During an external examination, you can notice the symptoms of chronic pancreatitis: the appearance of a symptom of red droplets - oval spots on the chest or abdomen, as well as pallor of the skin, dryness and flaking of the skin. Very often, patients with pancreatitis have ulcerations on the oral mucosa.
Any form of pancreatitis requires timely and high-quality treatment, since this pathology disrupts the digestion process and the removal of metabolic products from the body, which leads to complications and additional diseases.
Chronic enteritis often occurs in the form of chronic enterocolitis. Often chronic E. is the outcome of an acute one, but it can also occur independently.
A significant role in the development of the disease is played by infectious agents, protozoal and helminthic infestations, and nutritional factors (overeating, dry food, unbalanced in composition, for example, predominantly carbohydrate-rich or vitamin-deprived foods, abuse of spices).
General manifestations of the disease
are largely determined by impaired intestinal absorption. IN pathological process As a rule, other parts of the digestive system are involved.
There is a tendency to suppress the secretory acid function of the stomach, epigastric pain and dyspeptic disorders are noted; gastrobiopsy reveals gastric changes, in some cases - atrophic gastritis. A number of symptoms indicate damage to the pancreas (palpation pain, functional impairment).
In some cases, the liver is enlarged, its functions are impaired, and a biopsy reveals dystrophic changes in hepatocytes.
Of the common symptoms that attract attention
signs reminiscent of dumping syndrome, which may correspond to symptoms of hyperglycemia (immediately after eating - weakness, sudden heat in the head, feeling of a rush of blood to the head, palpitations, dizziness, hot sweat, redness of the face, copious amounts of thick saliva, nausea) or hypoglycemia ( the appearance, a few hours after eating, of severe weakness, dizziness, apathy, pallor, cold sweat, chills, sometimes flickering in the eyes, tinnitus). Increased fatigue, decreased performance, decreased appetite. Weight loss is observed with enteritis in 65-75%, sometimes it is quite significant.
A thorough examination of patients reveals a number of trophic disorders: dry skin, hair loss, increased brittleness of nails. Metabolism is disrupted. Protein metabolism disorders are indicated by hypoproteinemia, dysproteinemia, changes in the composition of blood amino acids, and hyperaminoaciduria. Disorders of lipid metabolism are confirmed by a decrease in lipids and their fractions in the blood serum.
In mild cases of the disease (grade I), the clinical manifestations are mild and local intestinal symptoms predominate.
With a disease of moderate severity (II degree), intestinal manifestations are significant, general disorders appear, which are not yet clearly expressed.
In severe cases (III degree), the general condition of the patients suffers significantly; the clinical picture is dominated by general symptoms.
Local intestinal symptoms:
bowel disorders, often diarrhea; bowel disturbances may be absent. An increase in the amount of feces (polyfecalia) is typical; remnants of undigested food are often visible to the naked eye; stool smears the toilet (steatorrhea). With diarrhea, stool is not very frequent, usually 4-6 times a day. Flatulence, often bloating is accompanied by an unpleasant taste in the mouth, lack of appetite, various painful sensations in the heart area, shortness of breath, headaches, sleep disorders, etc. Rumbling in the stomach, which, like flatulence, is most pronounced in the afternoon. Abdominal pain, mainly in the navel area, sometimes not localized throughout the abdomen.
When the disease is complicated by mesenteric lymphadenitis, the pain becomes constant and localized, intensifying with physical activity. Sometimes patients are bothered by a feeling of fullness and bloating immediately after eating. On examination, a distended abdomen is noticeable. On palpation, pain along the colon, pain at the so-called Porges point, to the left and slightly above the navel (in 44% of patients)
Causes of the disease may be ionizing radiation (radiation radiation), exposure to toxic substances (arsenic, lead, phosphorus), a number of medications (salicylates, indomethacin, corticosteroids, immunosuppressants, some antibiotics with prolonged or uncontrolled use). The disease may occur after gastrectomy or gastrectomy, vagotomy, gastroenteroanastomosis, or with atrophic gastritis. Chronic E. can develop against the background of chronic renal failure, diseases leading to tissue hypoxia (chronic nonspecific lung diseases, chronic heart diseases accompanied by chronic circulatory failure), eczema, psoriasis, food allergies, congenital or acquired enzymopathies. The cause of chronic E. may be wall ischemia small intestine, arising from atherosclerosis or inflammation of the mesenteric vessels (ischemic E.).
Morphologically, chronic E. is manifested by inflammatory and dysregenerative changes in the mucous membrane of the small intestine, and as the process progresses, its atrophy and sclerosis. The entire small intestine or its sections are affected.
The clinical picture of chronic E. consists of two symptom complexes, which should be considered as a manifestation of functional disorders associated with changes in the structure of the mucous membrane of the small intestine. One of them is caused by a violation of the processes of parietal (membrane) and cavity digestion. It is characterized by intestinal manifestations (local enteral syndrome): flatulence, abdominal pain, mainly in the middle part, loud rumbling, diarrhea, less often constipation or their alternation. On palpation, pain is noted in the middle part of the abdomen, as well as to the left and above the navel, at the level of the XII thoracic - I lumbar vertebrae (Porges symptom), “splashing noise” in the area of the cecum (Obraztsov symptom). The stool has a clayey appearance and is characterized by polyfecal matter.
Disorders of sexual function, biliary excretion, exocrine activity of the pancreas, etc. are noted. In chronic enteritis of grade I, intestinal symptoms dominate; Enteritis of the second degree of severity is characterized by a combination intestinal symptoms with mildly expressed metabolic disorders; with enteritis of the third degree, pronounced metabolic disorders prevail with the occurrence of often irreversible dystrophic changes internal organs. The symptoms of chronic enteritis in its late stage do not actually differ from the symptoms of other diseases that occur with malabsorption syndrome: celiac disease, exudative enteropathy, Crohn's disease, Whipple's disease, etc. Therefore, it is necessary to especially carefully examine patients with chronic enteritis of grade III severity to exclude these diseases.
A biochemical blood test reveals hypoproteinemia, hypoalbuminemia, a decrease in the blood serum levels of vitamins A, B2, B6, B12, C, D, E, K, P, folic acid, calcium, iron, phosphorus, magnesium, a number of microelements, cholesterol, phospholipids, beta-lipoproteins, glucose, etc.
Histological examination of the mucous membrane of the small intestine, obtained during intestinoscopy or aspiration biopsy, allows us to identify its inflammatory infiltration, dysregenerative and atrophic changes, and also to differentiate chronic E. from other diseases of the small intestine.
TREATMENT
Treatment for exacerbation of chronic E. is recommended to be carried out in a hospital. Bed rest is prescribed therapeutic nutrition.
In the first few days, food should be as chemically and mechanically gentle as possible, contain a lot of proteins, a limited amount of fats and carbohydrates (diet No. 4a). Avoid foods rich in fiber and whole milk.
In the future, the content of fats and carbohydrates is gradually increased (diet No. 4b). When the exacerbation subsides, food that is complete in the content of essential substances is allowed, which should remain gentle (diet No. 4c).
Drug therapy includes enzyme preparations, preferably not containing bile acids, and primarily pancreatin, trienzyme, orase, weak choleretic agents. To normalize stool, antidiarrheal drugs (imodium), astringents and enveloping agents, as well as infusions and decoctions of herbs (alder cones, bird cherry fruits, oak bark) are used.
For intestinal dysbiosis, it is prescribed in short courses medicines, affecting one or another microflora (with a predominance of staphylococcus - erythromycin, protea - nevigramon or furazolidone, fungi - nystatin, levorin), then biological preparations (colibacterin, bifidumbacterin, bificol, etc.).
Nitrosorbide, aminophylline, trental are used to stimulate intestinal absorption; to improve metabolic processes - methyluracil, pentoxyl, which simultaneously have an anti-inflammatory effect, for pain syndrome - substances with an antispasmodic effect (atropine, no-spa, halidor).
Drug correction of metabolic disorders is carried out with anabolic steroids: retabolil, methandrostenolone (Nerobol), as well as vitamins and folic acid; To eliminate electrolyte disturbances, potassium and sodium chloride, calcium gluconate, and magnesium sulfate are administered. In severe cases, intravenous infusions of amino acid mixtures and protein preparations are indicated.
Therapeutic enemas with astringents and adsorbents, antispastic drugs, antiseptics, and agents that enhance reparative processes are indicated. Drugs that normalize intestinal motility are prescribed depending on the nature of motor disorders. Mineral water is prescribed during the period of remission. For colitis with a tendency to constipation, waters such as Essentuki No. 17, Slavyanskaya, etc. are indicated, for a tendency to diarrhea - type Essentuki No. 4. For diarrhea, water is heated, for constipation, take water at room temperature.
Physiotherapeutic treatment: thermal procedures, mud therapy, electrical procedures, therapeutic exercises.
Prevention of chronic E. primarily includes timely treatment of acute intestinal diseases, balanced nutrition, and adherence to the regimen. It is also necessary to promptly identify and treat those diseases against which chronic E. occurs, and to avoid self-medication.
Enteritis in children can be acute and chronic. There are also special forms that occur with damage to both the small and large intestines - pseudomembranous enterocolitis and necrotizing enterocolitis of newborns. Acute E. in children usually occurs in the form of acute gastroenterocolitis. Chronic E. can be post-infectious, allergic, a consequence of enzyme deficiency, or post-operative. Often chronic E. is the outcome of acute. The main role in its pathogenesis, in addition to increasing the osmolarity of intestinal contents, intestinal hypersecretion and exudation, is played by the acceleration of the passage of intestinal contents and disruption of cavity and parietal digestion. The activity of many disaccharidases of the small intestine decreases early: lactase, invertase, maltase, etc. All types of metabolism are disrupted, the severity of which is the more significant, the more younger child and more severe illness.
The main local symptom is diarrhea. The stool is copious, light yellow in color, with pieces of undigested food, mixed with mucus. When fats are not digested, feces acquire a gray color, clayey appearance, and shine. The predominance of putrefactive processes causes the fetid odor of feces. At fermentation processes in the intestines, stool becomes foamy. Defecation is painful; during exacerbation, the frequency of stool reaches 10-20 times a day. Other signs of local enteric syndrome are also expressed: flatulence, rumbling, abdominal pain. On palpation of the abdomen, pain in the mesogastrium is determined, and positive Obraztsov and Porges symptoms are noted. General signs diseases are manifested by disorders of all types of metabolism and functional changes in other garfish and systems. E. is especially difficult in children younger age. They may develop disaccharidase deficiency and exudative enteropathy.
When making a diagnosis of chronic E., anamnesis (intolerance to certain foods, especially milk, information about intestinal infections), clinical manifestations (abdominal pain, rumbling, flatulence), stool character and results are important. scatological research. Investigate enzymatic, absorption and motor functions small intestine. An important role in diagnosis is played by intestinoscopy with targeted biopsy and subsequent morphological examination of biopsy samples of the mucous membrane of the small intestine. X-ray methods are not very informative and are unsafe for children.
The treatment is complex. A complete diet is prescribed with a 10-15% increase in protein content, a physiological amount of fat and a restriction of carbohydrates. Avoid foods containing large amounts of fiber, as well as whole milk (diet No. 4). The use of protein enpit and fermented milk lactobacterin enriched with lysozyme is effective. In severe cases use parenteral nutrition. Vitamins C, group B are administered, folic acid. The use of enzyme preparations (Pancreatin, Panzinorm, Polyzyme, Festal) is indicated. In severe cases of the process, antibacterial drugs are prescribed: derivatives of 8-hydroxyquinoline (enteroseptol), nitrofuran series (furadonin, furazolidone), nalidixic acid (nevigramon), as well as sulfasalazine and biseptol. After the course antibacterial treatment biological preparations that normalize intestinal microflora are indicated (colibacterin, bificol, lactobacterin, bifidumbacterin). Bacteriophages (staphylococcal, pseudomonas, coli-proteus, etc.) are also used. Enveloping and adsorbing agents are effective (tanalbin, white clay, bismuth preparations), medicinal plants(chamomile, peppermint, St. John's wort, nettle, blueberries, etc.). The prognosis for long-term treatment is favorable.
Primary prevention is aimed at identifying and actively monitoring children with dysbiosis, convalescents after acute intestinal infections, those suffering from functional intestinal disorders, food allergies. Secondary prevention involves early identification of children with E., their registration and observation. In spring and autumn, anti-relapse treatment is administered for a month (diet No. 4, vitamins, enzyme and biological preparations). In remission, but not earlier than after 3 months. after an exacerbation, sanatorium treatment is indicated at the resorts of Arzni, Caucasian Mineralnye Vody, Truskavets, Lake Shira, etc.
Pseudomembranous enterocolitis occurs during oral administration of antibiotics (usually lincomycin, clindamycin, ampicillin and especially cephalosporins). This is due to the increased proliferation of the enterotoxigenic strain Clostridiuni perfringens, which usually lives in the distal part of the intestine. Symptoms appear already in the 1st week of antibiotic therapy. Characterized by diarrhea, which is accompanied by abdominal pain, nausea, vomiting, and flatulence. The stools contain a lot of mucus and, less often, blood. In severe cases, the disease progresses violently, resembling an acute abdomen. The diagnosis is based on medical history, clinical manifestations, and the results of endoscopic examination. Sigmoidoscopy and colonofibroscopy make it possible to identify plaques and pseudomembranes consisting of mucus, fibrin, destroyed polymorphic and epithelial cells. In some cases, enterotoxin-producing clostridia are cultured from stool. Treatment includes mandatory withdrawal of antibiotics that caused enterocolitis and parenteral nutrition. Vancomycin is prescribed orally, to which clostridia are usually sensitive; Festal, Digital, and bacterial preparations are used, and detoxification therapy is carried out according to indications. If ineffective drug therapy, increasing intoxication, threat of intestinal perforation, one has to resort to surgical treatment. The prognosis with timely diagnosis and treatment is favorable, but with progression of the process it is serious.
Necrotizing enterocolitis of newborns is a serious disease accompanied by high mortality. Its etiology is unknown. Premature babies and low birth weight newborns are especially susceptible to the disease. Predisposing factors are intestinal ischemia and microcirculation disorders. The process is localized mainly in the distal small intestine and proximal large intestine. The resulting necrosis of the mucous membrane sometimes affects all layers of the intestinal wall, which leads to its perforation and peritonitis.
The disease usually develops in the 1st week of life, but can begin later - in the 2nd month. There is a sudden increase in the abdomen, and as a result of stagnation of food in the stomach, vomiting occurs, first periodically, then constantly. Intestinal peristalsis is enhanced, but absent with perforation. Profuse diarrhea appears, quickly leading to acidosis; the development of shock and disseminated intravascular coagulation is possible. The diagnosis is made based on the clinical picture, results X-ray examination. Plain radiographs reveal pneumatosis intestinalis: pneumoperitoneum indicates intestinal perforation. Microbiological examination of stool plays an important role for subsequent treatment. During treatment, the child is transferred to parenteral nutrition. Correction of disturbances in electrolyte balance, acid-base status, and blood coagulation system. Antibiotics (vancomycin, gentamicin) and oxygen therapy are prescribed. If there is no improvement in the child’s condition after 24-48 hours, as well as in case of intestinal perforation, it is indicated surgery- small bowel resection and ileostomy. The prognosis is serious.
The digestive system of a small child takes a long time to develop, so bowel problems before the age of one year are common. At the same time, there are various disorders, and sometimes there are such troubles as the appearance of food residues in the stool. This could be peels from plant foods, small parts of nuts, and much more. In this case, it is worth making allowance for the fact that the quality of the fruits and vegetables you purchase does not stand up to criticism. Moreover, if the act of defecation does not involve any unpleasant sensations, there is no reason to panic. You can avoid food particles in your child's stool by purchasing better quality products.
At the same time, there are certain signs that can reveal gastrointestinal tract disorders in a child. Such deviations include:
- the presence of mucous or blood impurities in the stool;
- pain during defecation;
- an abundance of intestinal sounds during intestinal peristalsis and much more.
The cause of such phenomena can also be an incorrect diet, especially if we're talking about about excessive amounts of fiber. It is important to know that food moves through the child’s gastrointestinal tract quite quickly, and there may not be enough enzymes capable of breaking down such substances. Then small lumps of undigested fiber may appear in the stool. In this case, there is also no serious reason for concern and treat the baby medical supplies no need. Such troubles can be eliminated by limiting the amount of plant foods in the diet.
The next problem that needs to be focused on is functional dyspepsia. The appearance of food particles in the stool is just one of the symptoms of this disease. Symptoms such as:
- Frequent belching.
- Decreased appetite.
- Loose stools.
- Mucous impurities in stool.
- Bloating, etc.
Among the reasons for such problems, one can note the mother’s refusal to follow a diet when feeding, lack of a diet, and too large portions when feeding. Also, such problems sometimes appear at the moment when the child begins to cut teeth or they are a consequence of taking certain medications. Also, to avoid troubles, do not rush to start feeding your baby food for which he is not yet functionally ready
Dysbacteriosis. It's a problem that adults can suffer from, but it's much more difficult for children. The fact is that when a baby is born, his intestines are sterile. It lacks both beneficial and harmful microflora. However, bacteria are colonized within several hours from the moment of birth. In this case, there may not be enough beneficial microorganisms. Such problems are manifested by changes in the color and consistency of stool, as well as possible appearance food particles due to intestinal disorders.
So, we have figured out the reasons for such phenomena, but what to do if they occur? We'll talk about this later.
How to correct digestive problems
We draw attention to the fact that medical assistance is not always needed. Of course, it would never be a bad idea to consult with a specialist, but in most cases the parents themselves are the culprits of the violations. Why is this so? We will talk about this in more detail.
First of all, when correcting digestive problems, the age and type of nutrition of the baby are important. Your child is on breastfeeding? This means that the mother needs to reconsider her own diet first. Professionals recommend following a special diet that will help you correct chemical composition breast milk. To do this, it is advised not to eat:
- foods with high fat content;
- fried foods;
- smoked meats
If none of this helped, or you strictly adhered to the specified diet and limited yourself in food, then most likely the problem lies in the child’s gastrointestinal tract. There is only one way out of the situation - see a doctor.
Often the appearance of food particles in feces is associated with the beginning of complementary feeding of the baby and accustoming him to solid or mushy foods. Indeed, bowel movements may become more frequent, and bowel movements may change. Perhaps it is simply too early for your child to eat such food, or you are feeding him too large pieces. Let us repeat, do not rush to start complementary feeding, and if such problems begin, postpone it for a month. Didn't help? Contact a specialist.
Don't overfeed your baby! Many parents often try to force-feed their baby, believing that he is not eating enough. Never try this! In infants, the gastrointestinal tract has not yet formed, and the stomach is small. Therefore, the baby himself knows how much food he needs in order to get enough. At the same time, overfeeding can lead to a whole range of all kinds of troubles.
Firstly, these should include overweight. The child should develop gradually; there is no need to try to speed up this process artificially. Secondly, you have a negative impact on the baby’s gastrointestinal tract, which is simply not ready to digest large volumes. In this case, not only violations may appear digestive system at a young age, and problems already at adult life. Be careful.
In general, we have listed the simplest situations that you can handle on your own. Feed your baby in adequate doses and on a schedule, then you can prevent huge amount digestive problems. However, there are situations in which the problem does not go away. It seems that you are following the diet, and you are avoiding complementary foods for now, and you are also not overfeeding. Please note that if any trouble occurs, you must contact a specialist!
Most people do not tend to carefully examine their own feces, and the design of modern plumbing often interferes with such research. If various kinds of impurities and inclusions are accidentally discovered in excrement, then it makes sense to be wary: some of them may be the first clinical manifestations of pathologies. Certain impurities are a good reason for visiting a doctor and further undergoing a medical examination, which necessarily includes testing.
Normal composition, color and consistency of stool
A healthy adult produces an average of 300 g of excrement per day, and defecation usually occurs once a day.
Please note:Normally, stool has an almost uniform consistency.
The main components of excrement are:

In the absence of acute and chronic diseases, as well as intestinal disorders, the color of adult stool varies from light brown to dark brown.
A change in color is one of the signs of the development of pathology. A greenish tint is one of the symptoms of regional enteritis (Crohn's disease), a gray color indicates problems with the pancreas, light gray or almost white indicates a violation of the functional activity of the liver (in particular, with Botkin's disease). A yellow tint indicates gallbladder disease.

What are the types of impurities?
The following impurities are most often detected in stool:
- leftover food;
- mucus;
- blood;
- foreign inclusions;
- pus.
The presence of impurities may indicate the development of diseases (sometimes quite serious pathologies of the digestive system), but it is often due to the nature of the diet.
Residues of food in stool
 If you find whole corn kernels or seeds (for example, sunflower seeds) in your feces, this is not a reason to sound the alarm. Some foods are very difficult to digest, especially if they are poorly chewed. Also, digestive enzymes are completely unable to cope with the veins present in meat products, as well as fish bones and fragments of eggshells.
If you find whole corn kernels or seeds (for example, sunflower seeds) in your feces, this is not a reason to sound the alarm. Some foods are very difficult to digest, especially if they are poorly chewed. Also, digestive enzymes are completely unable to cope with the veins present in meat products, as well as fish bones and fragments of eggshells.
The reason for a visit to the doctor is the presence of undigested meat fibers, as well as cottage cheese or eggs, in the excrement. This sign indicates a lack of digestive enzymes.
Please note:the presence of large particles of undigested food is called lientorrhea. When meat fibers are detected, they speak of creatorrhoea.
The reason for the lack of enzymes may be:
- insufficient secretion of pancreatic juice (after resection of part of the pancreas or against the background of pancreatitis);
- inhibition of enzyme secretion in the intestine;
- pronounced atrophy of the gastric mucosa.
Residues of food may appear in the stool during its accelerated evacuation against the background of increased peristalsis. In this case, some foods simply do not have time to be digested and absorbed. This phenomenon is particularly characteristic of irritable bowel syndrome.
If the stool has an oily sheen, this is a sign of steatorrhea, i.e. the presence of a large amount of lipid compounds (fats).
Possible causes of steatorrhea:
- a large amount of fat in the diet;
- diseases of the liver, gall bladder and ducts (cirrhosis, hepatitis, cholecystitis, etc.);
- pancreatic diseases (inflammation, strictures, ulcers and tumors);
- hemochromatosis (accumulation of iron in organs due to metabolic disorders);
- intestinal pathologies (inflammatory, autoimmune and tumor);
- endocrine diseases and pathologies of the endocrine glands;
- congenital (hereditary) diseases;
- systemic manifestations of skin diseases;
- Excessive consumption of laxatives.
Mucus in stool
 Please note:the presence of some mucus in the stool (in the form of lumps or inclusions) is normal for children early age who are breastfed. Mother's milk is characterized by high fat content, which the baby's digestive enzymes are not yet able to fully cope with.
Please note:the presence of some mucus in the stool (in the form of lumps or inclusions) is normal for children early age who are breastfed. Mother's milk is characterized by high fat content, which the baby's digestive enzymes are not yet able to fully cope with.
Anyone healthy person cells of the intestinal wall produce mucus, which is necessary to facilitate the passage of stool through the lower parts of the digestive tract. A small amount of colorless (almost transparent) mucus is often normal and is not a cause for concern.
If mucus is released in large volumes or is brown or yellowish in color, this may indicate the following pathologies:
- increased intestinal motility;
- inflammatory diseases of non-infectious origin;
- acute intestinal infections (dysentery, typhoid fever, etc.);
- benign or malignant formations;
Please note:often a large amount of mucus is the first clinical sign development of regional enteritis (). The admixture of a significant amount of mucus is also quite often recorded in chronic constipation.
Based on the degree of distribution of the mucous component in feces, the height of the location of the pathological focus can be determined. If mucus relatively evenly permeates the excrement, then the inflammatory process is localized in the upper sections of the intestine, but if impurities are detected on the surface (usually in the form of lumps), then the lower sections are affected.
Bloody feces
The presence of blood in excrement is an absolute reason to consult a doctor, since it can be a clinical manifestation of the following diseases:
- autoimmune intestinal pathologies ();
- malignant neoplasms of the gastrointestinal tract;
- benign tumors of the intestinal walls ();
- ischemic colitis;
- diseases of infectious origin (dysentery, etc.);
- and ulcers of the rectum and rectal area;
- intestinal angiodysplasia;
- blood pathologies (clotting disorders);
- some helminthic infestations (in particular, ascariasis).
Blood volume varies depending on the nature of the disease and the severity of the pathology. Feces often contain only small and inconspicuous streaks, but in case of serious pathologies, up to 200 ml or more can be released during defecation. In this case we are talking about intestinal bleeding, which requires immediate action.
 Please note:in some pathologies, during the act of defecation, only blood mixed with intestinal mucus is released.
Please note:in some pathologies, during the act of defecation, only blood mixed with intestinal mucus is released.
The color of blood in the stool makes it possible to determine with a high degree of probability the approximate location of the bleeding site. The scarlet color and location of the blood on top of the feces indicates that there is a pathology of the sigmoid, descending or rectum. Fresh blood is also released from cracks anus and hemorrhoids. More dark blood and blood clots mixed relatively evenly with the stool indicate that the source of bleeding is in the upper parts of the large intestine (colon) or in small intestine. Black coloring of the stool may indicate that blood is being secreted in the stomach or esophagus (the specific color is due to the fact that the blood has been exposed to hydrochloric acid of the gastric juice).
Please note:a reddish tint to the stool or burgundy streaks are not always due to the presence of blood - be sure to remember if you ate beets the day before?
Foreign inclusions
The presence of films in feces may be due to a rather serious pathology of the large intestine - pseudomembranous colitis, often caused by long-term or irrational antibiotic therapy.
Fragments of necrotic tissue are found during decay malignant tumors, as well as with intussusception due to intestinal obstruction.
Upon admission pharmacological drugs in granular forms, their particles are also often detected in the stool. Activated carbon gives excrement a black color.
The so-called feces are sometimes detected. pancreatic, biliary and intestinal stone formations - coprolites. Intestinal compactions (stones) are not true stones, but are highly compacted feces formed due to chronic constipation. This pathology is more typical for elderly patients. True coprolites consist of an organic core with gradually growing mineral salts. The presence of such stones in the stool suggests diseases of the pancreas or bile ducts.
Pus in stool
The presence of pus in feces is unconditional evidence of the development of a pathology of inflammatory origin. In most cases, pus is detected in parallel with blood and mucus.
Pus may have a yellowish or greenish tint and appears in the following diseases:
- proctitis;
- infectious colitis;
- ulcerative colitis;
- decay (in the later stages of cancer);
- breakthrough of an abscess into the intestinal lumen;
- autoimmune intestinal damage (Crohn's disease).
Important:remember that if pus is released during defecation, then self-medication is strictly unacceptable. ABOUT positive effect in this case there is no question.
Treatment
The detection of most of the mentioned impurities is the basis for contacting a gastroenterologist at the clinic. The local physician can also refer the patient to a specialized specialist and prescribe a series of tests.
Specialists whose consultation may be needed:
- proctologist;
- infectious disease specialist;
- surgeon;
- hematologist;
- oncologist.
Important:with the release of a large amount of blood against the background of deterioration general condition, you should call an ambulance. Massive bleeding is a life-threatening condition and requires hospitalization of the patient in the intensive care unit or intensive care unit.
To establish or clarify the diagnosis, in most cases the patient is referred for examination to an endoscopist.
Plisov Vladimir, medical observer

There are two generally accepted methods for assessing stool: macroscopy and microscopy. Macroscopic examination evaluates the visual characteristics of feces, and microscopic examination evaluates its initial data under a microscope.
Laboratory assistant during...
0 0
2
It's no secret that the main indicator of human health is normal tests, which should have a certain appearance, smell and condition. First of all, we are talking about feces and urine. Of course, if, for example, the consistency of a child’s feces is disturbed, this is already a reason for the mother to sound the alarm. The same reaction will follow if the baby has undigested food in his stool. Naturally, this disease is typical not only for children, but also for adults, so it requires the most detailed consideration. So, let's try to figure out why undigested food appears in the stool, and how this problem can be eliminated.
What to remember
If we talk about an adult, then feces should have a uniform consistency and color, without any inclusions, including lumps, particles of blood, mucus, and especially food.
When visiting the toilet, it would be a good idea to check from time to time appearance bowel movements. If undigested...
0 0
3
Undigested food in the stool of children: why and what to do
Stool disorders in a one-year-old child, unfortunately, are not uncommon, but what to do if undigested food particles appear in the stool? Such phenomena do happen and often become a cause of concern for new mothers. Experts often devote entire programs to bowel movements in children, for example, Dr. Komarovsky is one of them.
The saddest thing is that in most cases, it is the parents who are to blame for such violations, due to excessive efforts to “do everything for the baby.” Although there are also problems that require drug treatment, in such cases, contacting a specialist is mandatory! Today we’ll talk about why there are undigested food residues in a child’s stool and what to do in such a situation.
Causes of the problem
The digestive system of a small child takes a long time to develop, so bowel problems before the age of one year are common. At the same time...
0 0
4
The appearance of undigested food debris in the stool of an adult may be the result of an upset stomach, infectious disease or constipation.
But most often this is not a pathology - some types of fiber are simply not completely absorbed by the body, and this is the norm for it. In other cases, a healthy person should not experience lumps or pieces of undigested food during bowel movements.
What could be the causes of this problem?
Several types of fiber are intended for human consumption plant origin– digestible and indigestible. Each of these species can be found in stool after the act of defecation.
Digestible fiber. If it is observed in the stool, this indicates a lack of hydrochloric acid in the body, which is responsible for the breakdown of cells.
A low level of acidity causes pieces of fruits and vegetables to remain in the stool. Usually these are particles of carrots, potato tubers,...
0 0
5
The digestive tract is the most voluminous system of the body and many indications of a person’s health depend on its work.
The modern lifestyle and the amount of varied, not always healthy, food lead to the fact that people are increasingly experiencing various disorders of the digestive tract, and one of them is undigested food in the feces of an adult.
The causes of this pathology
With the normal functioning of the intestines, food entering the stomach is completely broken down and then excreted from the body. In this case, there should not be any individual undigested pieces of food. The only exceptions are products that were obviously not intended for this purpose: fruit seeds, pits, and foreign bodies.
The presence of undigested pieces in stool may indicate the following problems:
Impaired functioning of the pancreas, insufficient amount of gastric juice or changes...
0 0
6
Hello! Undigested pieces of food in the stool of an adult may indicate: 1. Pancreatic insufficiency, 2. Insufficient secretion of hydrochloric acid in the stomach, 3. Accelerated evacuation of food from the gastrointestinal tract (often accompanied by diarrhea). To clarify the diagnosis, an examination by a gastroenterologist and further examination are necessary: FGDS, General analysis blood, complete blood test (ALT, AST, alkaline phosphatase, total bilirubin + fractions, glucose, cholesterol, amylase), elastase 1 in feces, coprogram. If the cause is pancreatic insufficiency, then enzyme preparations (Pancreatin, Creon, Mezim, etc.) are prescribed. If the reason lies in low stomach acidity, then under the supervision of a gastroenterologist it is necessary to be examined for Helicobacter pylori (there are several diagnostic methods: breath test for H. pylori, stool test for H. pylori (PCR), antibodies to H. pylori). In the absence of bacteria, they take secretory activity stimulants (Pentagastrin, etc.) or...
0 0
7
Many mothers, having discovered undigested pieces of food in their child’s stool, begin to worry greatly and are right to do so! The baby’s body (including the digestive system) is imperfect at birth. Many systems are, roughly speaking, not fully developed. Enzymes are produced in insufficient quantities. The intestines, liver and pancreas cannot cope with the food usual for an adult. That is why pediatricians monitor the nutrition of children under one year so strictly.
What does undigested food in a child’s stool mean?
If the child does not have a congenital pathology of the digestive system, it is excluded intestinal infection, there is no mucus, “green” or unpleasant odor, then undigested pieces of food in the stool may indicate functional dyspepsia or pancreatopathy. This insufficiency of the intestines and pancreas, respectively, is a very common occurrence today, which is associated with a violation of the diet in children of the first year of life.
During the first year of a child’s life, all organs and...
0 0
8
Response: In order to accurately pay for this demand, it’s okay to analyze the stool for coprogram. This analysis allows us to identify dysfunctions of the gastrointestinal tract, liver, pancreas, the presence of close movement of food through the stomach and intestines, and diagnose inflammatory processes in the digestive tract, and also helps to identify helminths in the intestines. Well, as both treatment and prevention, I advise you to take the highest quality pumpkin oil at dawn on an empty stomach. For a 2.5 year old child, 2-3 particles are enough. You can take up to six moons and all digestive processes will normalize. Then analyze it again or check the appearance of the stool.
Read...
0 0
9
Changes in the appearance of stool
Many people know firsthand about changes in the color, smell and consistency of stool, because every person has encountered such concepts as diarrhea, intestinal disorders or infections, constipation at least once in their life. But undigested food in an adult’s stool can cause real panic for some. In normal condition, feces should not contain any inclusions, lumps or pieces of undigested food, mucus, blood and...
0 0
10
Standard laboratory tests often provide sufficiently voluminous information about the patient’s health status. Such analyzes not only show how correctly or incorrectly the body functions, but also help to identify what exactly the essence of the violations is. A fairly popular study is considered to be a coprogram - a study of the characteristics of feces. When carrying out such an analysis, plant fiber that is indigestible in feces may be identified; such a disorder can be observed in both a child and an adult; we will consider its causes and talk about what to do in this condition.
Plant fiber is indigestible in a child’s stool
Normally, in completely healthy children, small particles of undigested coarse food products, such as nuts, peels of vegetables and fruits, can be periodically observed in the stool. It may well be that the food was of poor quality. At the same time, experts say that if the child does not feel unwell...
0 0
11
Who's talking about what, and I'm talking about again
poop. If you find it unpleasant to read, you can immediately pass by. In general, my son has chronic constipation, dolichosigma is in question. Gastroenterologist
The clinic sends me for an x-ray without prescribing any additional tests.
He says that if the X-ray doesn’t confirm then we’ll take tests and look
another reason. Of course, I don’t agree with this, I’m not ready to send the child
for X-ray (which is done under
anesthesia). We decided to get all the tests done first and consult with someone else
doctor, and then only if anything
will do an x-ray. We only made an appointment with the doctor on August 20th, earlier there was no appointment at all.
Can’t get an appointment, make an appointment a month in advance (but the doctor’s reviews are very
good). We are still getting tested. Done
Ultrasound of the gastrointestinal tract, everything is fine there. Today
We took a copagram test. And then I noticed that in the child’s stool very often
sometimes there are a lot of pieces of undigested food, could this be the reason...
0 0
12
The proper functioning of the digestive system is the basis for the normal functioning of both men and women. female body. However, the modern lifestyle of most urban residents is not conducive to stomach and intestinal health. Undigested food in the stool of an adult and other dyspeptic disorders are increasingly becoming a reason to quickly consult a doctor.
What can particles of undigested food in stool indicate?
Normally, the internal environment of the digestive system is capable of breaking down the vast majority of substances that enter it. An exception in this case may be solid particles that were not originally intended for food (fruit seeds, foreign bodies). Undigested food in an adult's stool can be a sign of several gastrointestinal diseases.
Pancreatic insufficiency Insufficiency of gastric juice Accelerated evacuation of food from the gastrointestinal tract. In this case, the food simply does not have time to undergo the processes...
0 0
13
» Causes and treatment
Indigestion of food causes in adults treatmentUndigested food in the stool of an adult: causes, norm, concomitant diseases
The functioning of the digestive system can be judged not only by certain sensations in the stomach or intestines, but also by the appearance, smell and color of feces. Most often, such studies are carried out by young mothers, for whom newborn feces are perhaps the most important indicator of the health of their children. But adults also have a lot to learn from inquisitive mothers, especially if certain changes were noticed in the stool.
Changes in the appearance of stool
Many people know firsthand about changes in the color, smell and consistency of stool, because every person has encountered such concepts as diarrhea, intestinal disorders or infections, constipation at least once in their life. But undigested food in an adult’s stool can cause real panic for some. In normal condition, feces are not...
0 0
14
Everything will be fine!
Of course, go to the doctor for peace of mind, but, in my opinion, don’t get hooked on pills.
And we also had a lot of carrots. By the way, some mothers told me that carrots are in their children’s feces, so for some reason this is such a product. :) Remove it, and then introduce it drop by drop.
And since you still have breastfeeding, don’t worry about your child getting enough to eat, believe me, milk still contains a lot of useful things and the child will not go hungry. But, try to adjust the hot water mode. As they told me, if a child eats a normal portion of such food, and then also drinks milk, then the portion will be too large, and this is bad for the pancreas. In general, eat no more than 200 grams at a time. Try to control it. It's hard, but you can do it! And it's okay! :)
Health to you and...
0 0
