Changes in the retina of the eye symptoms. Changes in the retina with collagenosis. Peripheral retinal dystrophy - classification and general characteristics of types.
Eye health
Retina of the eye - diseases, causes and symptoms, treatment
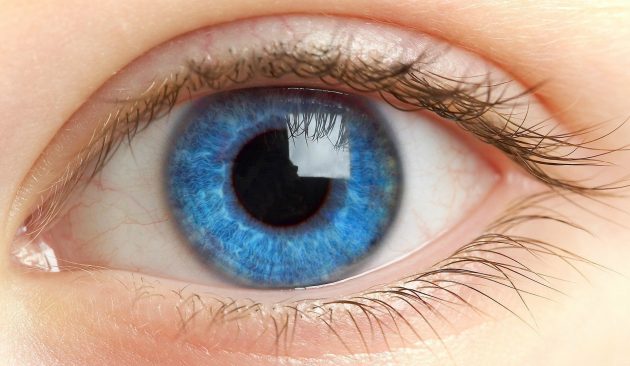
 The retina of the eye plays one of the most important roles in visual perception environment. It is the inner sensitive membrane of the eye, which performs the function of receiving light and color signals, and then delivering them through the optic nerve to the brain.
The retina of the eye plays one of the most important roles in visual perception environment. It is the inner sensitive membrane of the eye, which performs the function of receiving light and color signals, and then delivering them through the optic nerve to the brain.
Remember, it is important to identify any changes in yourself and any symptoms and promptly seek appropriate advice. medical care to maintain good visual health. And you, how do you look after your eyes? The specified content is the responsibility of the author and reflects his point of view, but not the ideology of the site.
It is usually more common in people who are nearsighted or those who have previously had a retinal disorder. Retinal detachment can be a severe blow. Less commonly, it is associated with hereditary diseases, so it can also occur in children. Treatment should not be delayed as this may lead to deterioration or permanent loss of vision. The retina is a thin, transparent membrane formed by a series of layers of fibers and light-sensitive cells, and is actually an extension of the brain.
However, for certain reasons, the retina, as well as other constituent elements of the visual organs, may undergo pathological changes. Diseases of the retina if not treated promptly can lead to various serious consequences, in particular to a severe decrease in visual acuity and its breakup.
 Among the reasons that provoke the development of retinal diseases, it is worth highlighting the hereditary factor. Pathological changes in older age can also be explained by birth injuries and congenital anomalies themselves.
Among the reasons that provoke the development of retinal diseases, it is worth highlighting the hereditary factor. Pathological changes in older age can also be explained by birth injuries and congenital anomalies themselves.
The retina covers the inside of the eye, just as the paper in a room covers the walls. The function of the retina is similar to that of photographic film: light passes through the cornea and lens and is focused on the retina. The light stimulates the cells in the retina, which are responsible for “image capture” and turn the light stimulus into an electrical stimulus that will travel through the optics to the brain, where we have the sensation of vision.
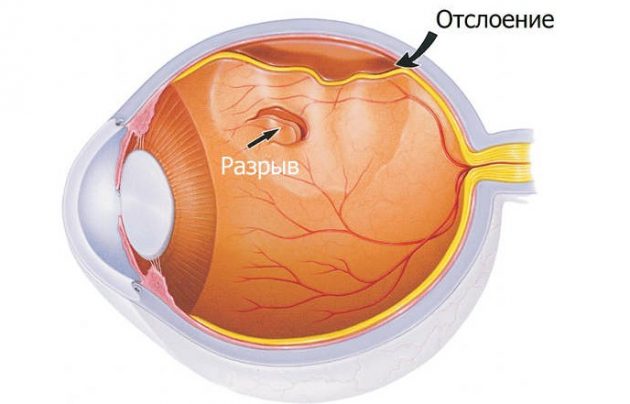
Most retinal detachments are caused by bleeding or tears in the retinal tissue structure. Inside the eyes is a glassy humor that is firmly attached to the retina at certain points. Vitreous traction can cause a tear or hole in the retina. Although some glassy deposits occur naturally with aging and do not cause damage to the retina, abnormal eye growth, inflammation, or accidents with eye trauma can cause glassy peeling. In most cases, significant change in the vitreous structure can occur before retinal detachment.
Most often, retinal diseases occur as a result of:
- Circulatory disorders
- Eye diseases and inflammatory processes,
- Not eye diseases(against the background of diabetes, hypertension, atherosclerosis, rheumatism, etc.).
- Injuries of the organs of vision and craniocerebral.
- Prolonged stressful situations and surgical interventions.
Against the background of the listed reasons due to which retinal diseases occur, we can conclude that they are secondary. In other words, most retinal diseases develop on the basis of existing pathological processes and are thus their complication.
First, a tear appears in the retina, through which vitreous fluid penetrates, facilitating retinal separation and subsequent detachment. The area of the retina that is severed cannot function properly and will cause blurred vision or complete blindness or part of the visual field depending on the extent of the detachment.
It should be noted that there are some retinal detachments caused by other eye conditions, such as tumors, severe inflammation, or complications of diabetes. These are called secondary retinal detachments, in which there are no tears or holes in the retina, and treating the condition that caused the retinal detachment is the only therapy that allows the retina to return to its normal position.
 It is noteworthy that on initial stage development of the pathological process, symptoms may be completely absent or not significant at all. At the same time, the symptoms of most retinal diseases are similar to those of other diseases of the organs of vision.
It is noteworthy that on initial stage development of the pathological process, symptoms may be completely absent or not significant at all. At the same time, the symptoms of most retinal diseases are similar to those of other diseases of the organs of vision.
ABOUT The main symptoms of retinal diseases:
An eye examination by an ophthalmologist is necessary to analyze the internal structures of the eye and determine the presence of retinal detachment. The exam should be performed as soon as the first symptoms appear because a recent retinal detachment can be treated surgically before a more serious and irreversible situation occurs.
Some retinal detachments may be initiated without the presence of floaters or flashes of light. In these cases, patients may notice a pulsation or fog in their vision or the appearance of a shadow in the lateral areas of the visual field. The development of a retinal detachment will cause blur in central vision and create significant vision loss if treatment is not treated quickly and effectively.
- Disorientation when poor lighting and in dark period days.
- Decreased visual acuity, accompanied by the development of moderate and severe myopia.
- The appearance of a “veil” before the eyes and a distorted perception of the environment.
- Double vision, the appearance of “flashes, spots and lightning.”
- Narrowing of the field of view. Basically, restricting the inspection of objects from side to side.
- Some fragments also fall out, most often on the sides.
- Loss of central vision.
- Change in color perception.
These symptoms are often accompanied by other signs. People with retinal diseases may experience high blood pressure, a bulging sensation, migraines, and darkening of the eyes.
Sometimes, retinal detachment can occur suddenly and the patient may experience complete loss of vision in one eye. This sudden loss of vision can also be caused by vitreous hemorrhage associated with a retinal tear or detachment. Preventive or preventive treatment aims to control all these injuries or tears that can lead to retinal detachment. Among the possible preventive treatment methods, we highlight cryotherapy and laser photocoagulation.
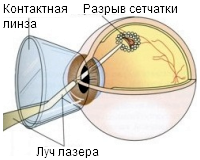
Photocoagulation consists of giving a series of laser hits to any lesions that may predispose to retinal detachment. The laser will seal the retina in areas where it is weakened, creating strong adhesion between the layers of the retina. This is a painless process and is done through the student.
 It should be noted that most often retinal diseases occur in middle-aged and elderly people. In very rare cases they are diagnosed at a young age.
It should be noted that most often retinal diseases occur in middle-aged and elderly people. In very rare cases they are diagnosed at a young age.
The group of common retinal diseases includes:
- Dystrophic, which, depending on the affected area, are central and peripheral. Depending on the form of acquisition - hereditary and acquired throughout life. The first type of dystrophic diseases includes pigmentary dystrophy, and the second - chorioretinal, macular.
- Angiopathy, which comes in several types : hypertensive, hypotonic, juvenile, diabetic and traumatic. Following the names, we can conclude that this disease is truly secondary. It occurs due to defeat blood vessels and manifests itself, depending on the type, as spasm or dystonia.
There are also other pathological processes in the retina. For example:
Cryotherapy is also designed to seal existing lesions, but is performed by applying a cold probe to the outer wall eyeball. However, in some cases, retinal detachment has already occurred and we must resort to curative treatment. Scleral or classical surgery involves the placement of explants to deepen the wall of the eyeball inwards. This brings the wall closer to the individual retina, facilitating retinal tear packing and retinal adhesion to the eye wall.
Usually usually combined with laser. Vitrectomy is another type therapeutic therapy, characteristic of those cases when retinal detachment occurs as a result of the action of the vitreous body. The vitreous causing the lesion will be removed and emptied and replaced by an injection of a substitute that penetrates the ocular substances such as air or expansive gases or silicone oils to press on the retina and adhere properly. Laser lesions or tears have been treated previously.
- Retinitis, which is an inflammatory process. It can occur in one eye or after a while in both eyes. Provoke its occurrence various diseases, including viral and venereal (syphilis). It often occurs against the background of toxic damage to the body and an allergic reaction.
- Neoplasms that can be benign or malignant. Experts say that their occurrence in 90 percent of cases is associated with poor heredity. However, it is possible that they can appear as a result of inflammatory processes and for any other reasons.
Unfortunately, in most cases the diseases are asymptomatic, and they can only be diagnosed when complications arise. A complication of all such diseases is a rupture of the retina and its gradual detachment.
Finally, we can also use gas injection, but without removing the vitreous. In this case, a gas bubble is introduced, which presses on the affected retina and facilitates its adhesion. Later it will also be completed with cryotherapy or laser. Early detection of injury to the back of the eye that can lead to retinal detachment is the best defense against vision loss. Even when symptoms are not observed, periodic screening is recommended, especially for those at risk.
It is important to remember that retinal detachment is not painful and requires immediate treatment. The macula is a small area of the retina located in the center of the visual axis that is responsible for fine vision, which is used in reading, drawing, and detailing.
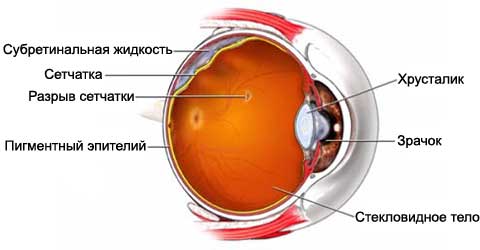 Retinal tears are pathological disorders that are accompanied by partial and then complete tissue detachment. In places where tissue detachment occurs, liquid leaks out. For this reason, there is a gradual, in some cases sharp, decrease in visual acuity.
Retinal tears are pathological disorders that are accompanied by partial and then complete tissue detachment. In places where tissue detachment occurs, liquid leaks out. For this reason, there is a gradual, in some cases sharp, decrease in visual acuity.
The remaining retina is called the peripheral retina: it is responsible for vision in low visibility conditions and is very useful for identifying possible less central obstructions in our field of vision. Age-related degeneration Macula has been the most common cause of irreversible vision loss for over 50 years in developed countries.
This condition does not cause complete blindness, but makes reading and observing details very difficult without the use of magnification systems. On the other hand, the patient will be able to move and avoid obstacles that appear along the way. This disease is age-related and can occur from the age of 50 and then gradually becomes more common.
There are several types of retinal tears:
- Macular, arising due to fusion of the vitreous body directly with the retina in the macula area. Macular holes form in the central part of the retina.
- Valve valves are caused by the same reason as the previous ones. However, in this case, retinal tears can be provoked by pathological changes in the vitreous body, namely its detachment.
- Along the jagged line. The reasons for this situation are serious injuries eyes and heads.
- Hole-like, caused by peripheral dystrophies of the retina, which lead to its tight fusion with the vitreous body.
The main causes of retinal tears are excessive eye and physical stress, increased blood pressure, prolonged stressful situations and head injuries, directly to the eyes.
The retina, and therefore the macula, lies on a layer of blood vessels that supplies them with oxygen and nutrients and removes the products resulting from their activity. Over time, changes begin to appear in the macula itself, with the destruction of its cells and subsequent loss of vision.
Sometimes abnormal vessels initiate migration into the retina, resulting in urine or neovascular disease. The wet form has a faster and more severe evolution than the dry form. Fortunately, it is also less common. Patients who have these abnormal vessels in one eye have a 50-90% risk of this complication in the other eye.
The symptoms of this pathological process are similar to the manifestations of retinal diseases. However, it has a sharper and more pronounced character.
Signs of ruptures appear as if from nowhere. This:
- “flashes, lightning and veils” before and in the eyes,
- impairment of central or peripheral vision,
- a sharp drop in visual acuity,
- loss of fragments from the field of view and its limitation.
It is noteworthy that these symptoms can also characterize retinal detachment that has already begun. Therefore, if at least one of the symptoms occurs, you must immediately seek help from an ophthalmologist.
We only have therapeutic weapons that help prevent, stop or delay disease. Many studies demonstrate the importance of xanthophyll carotenoids such as lutein and zeaxanthin in the macula as essential for protection against light-induced oxidation.
Recent research indicates a synergistic effect between lutein and omega. In the wet form of the disease can be performed laser treatment, photodynamic therapy or injection of substances that prevent the growth of abnormal blood vessels. You can even combat risk factors such as tobacco and unprotected light.
 Alas, retinal diseases are often diagnosed in late stages. As a result, surgical intervention becomes the way to cure them.
Alas, retinal diseases are often diagnosed in late stages. As a result, surgical intervention becomes the way to cure them.
If some of them are identified at the initial stages, it is quite possible to slow down their development process with the help of special injections. Depending on the nature of the disease, these may be antibiotics, vasoconstrictors or dilatants. eye drops(hypo- or hypertensive type of angiopathy), etc.
Balance blood pressure Treatment regimen and anticholesterol sun protection. . To combat oxidative stress, it is important to maintain a rich and varied diet. If your diet is insufficient or unbalanced, you can take a supplement with vitamins, minerals, antioxidants, lutein and omegas.
Contact an ophthalmologist! Vascular retinopathy include hypertensive retinopathy, diabetic retinopathy, central reticular artery occlusion and central retina. Hypertensive retinopathy occurs with significant chronic hypertension, malignant hypertension and severe toxemia. It develops from hypertensive arteriosclerosis, which is the thickening of arterioles in response to chronic hypertension. These sclerotic changes lead to the fact that the light reflex of the arteriole becomes wider and weaker.
Laser treatment or strengthening the retina using laser coagulation is the best alternative to other methods. Using a laser, you can “strengthen” and prevent retinal detachment in the peripheral or central part. It is noteworthy that the use of this type of treatment is possible for degenerative and dystrophic changes, thrombosis, angiopathy and other diseases.
On early stages Hypertensive retinopathy of the fundus has a generalized or focal narrowing of the retinal arterioles. As the disease progresses, superficial hemorrhages appear as “candle flames” and small white superficial areas of retinal ischemia. Another visible change, but later, is yellowish hard exudates resulting from the deposition of lipids in the deeper layers of the retina, which occurs in the extravasation of retinal vessels, as observed later. These hard exudates may form a star-shaped pattern around the macula.
Laser intervention occurs within 15-20 minutes, during which the eyeball is not opened. During the operation, only local anesthesia is required and after a couple of hours the patient can go home. Recovery period as such – no. But ophthalmologists recommend not to strain your eyes, not to be in the sun for a long time and to follow the rules of hygiene.
The optic disc becomes congested and swollen in severe hypertension. Treatment of Hypertensive retinopathy and arteriosclerosis can only be controlled by clinical treatment hypertension. This leading cause of blindness can be especially severe in people with insulin-dependent diabetes mellitus, but it is also common in chronic non-insulin-dependent diabetes mellitus. The degree of retinopathy is closely related to the duration of diabetes.
Nonproliferative retinopathy is characterized by increased capillary permeability, microaneurysms, hemorrhages, exudates and edema. Patients usually do not exhibit visual symptoms in the early stages of nonproliferative retinopathy. Pregnant patients with diabetes should be tested every trimester during pregnancy.
There are two types of surgical intervention in the retina: extrascleral and endovitreal. The first type of intervention occurs on the eyeball, and the second - directly in it. Regardless of this, the goal of both types of surgical interventions is to maximize the reunification of the retina with the pigment epithelium.
During the operation, the so-called filling of the detached areas of the retina occurs. In some cases, ballooning is possible. In other words, a special catheter with a balloon is temporarily sutured at the site of the rupture. It applies the same pressure as during filling.
However, both surgical intervention and laser coagulation have a number of indications and contraindications. Unfortunately, even after them, it is possible that negative consequences and complications such as relapse, prolapse upper eyelid etc. The ophthalmologist must warn about the positive and negative aspects. Be healthy!
Video
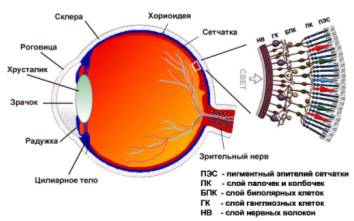
The retina of the eye is the initial section of the visual analyzer, which ensures the perception of light waves, their transformation into nerve impulses and transmission to the optic nerve. Photoreception is one of the most important and complex processes that allows a person to see the world around him.
Today, retinal pathology is a pressing problem in ophthalmology. Diabetic retinopathy, acute obstruction of the central artery, various retinal and retinal detachments are common reasons irreversible blindness in developed countries.
Anomalies in the structure of the retina are associated with, night blindness(poor room lighting prevents a person from seeing normally) and some other visual disorders. Knowledge of the anatomy and physiology of the retina is necessary to understand the mechanism of development in it pathological processes, principles of their treatment and prevention.
What is the retina
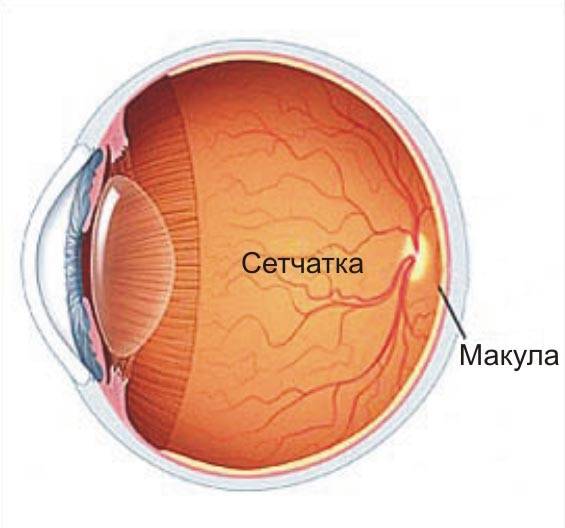
The retina is the inner layer of the eye, lining the inside of the eyeball. Inwardly from it is the vitreous body, outwardly - the choroid. The retina is very thin - normally its thickness is only 281 microns. It should be noted that in the macula area it is slightly thinner than at the periphery. Its area is about 1206 mm 2.
The retina lines approximately ¾ of the inner surface of the eyeball. It stretches from the optic disc to the dentate line, where it passes into the pigment epithelium and lines the ciliary body and iris from the inside. At the dentate line and optic disc, the retina is attached very firmly; in all other places it is loosely connected to the pigment epithelium, separating it from the choroid. It is the absence of a tight connection that causes such easy development of retinal detachments.
The layers of the retina have different structures and functions, but together they form a complex structure. It is thanks to the close contact and interaction of various parts of the visual analyzer that people are able to distinguish colors, see surrounding objects and determine their sizes, estimate distances, and adequately perceive the world around them.
Entering the eye, the incoming rays pass through all its refractive media - the cornea, chamber humor, lens, vitreous body. Thanks to this, in people with normal refraction, the image of surrounding objects is focused on the retina - reduced and inverted. Subsequently, the light impulses are transformed and enter the brain, where the picture that a person sees is formed.
Functions
The main function of the retina is photoreception - a chain of biochemical reactions during which light stimuli are converted into nerve impulses. This occurs due to the breakdown of rhodopsin and iodopsin - visual pigments formed when there is a sufficient amount of vitamin A in the body.
The retina of the eye provides:
- Central vision . Allows a person to read, do close-up work, and clearly see objects located at different distances. The cones of the retina, which are located in the area of the macula, are responsible for it.
- Peripheral vision . Necessary for orientation in space. It is provided by rods, which are localized paracentrally and on the periphery of the retina.
- Color vision . Makes it possible to distinguish colors and their shades. Three different types of cones are responsible for it, each of which perceives light waves a certain length. This enables a person to distinguish between green, red and blue colors. Impaired color vision is called color blindness. Some people experience a phenomenon called a fourth, extra cone. It is typical for 2% of women who can distinguish up to 100 million colors.
- Night vision . Provides the ability to see in low light conditions. It is carried out thanks to rods, since cones do not function in the dark.
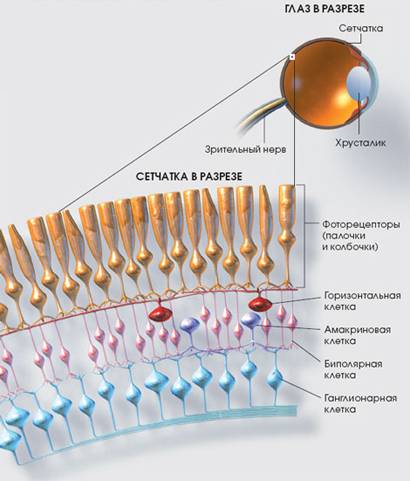
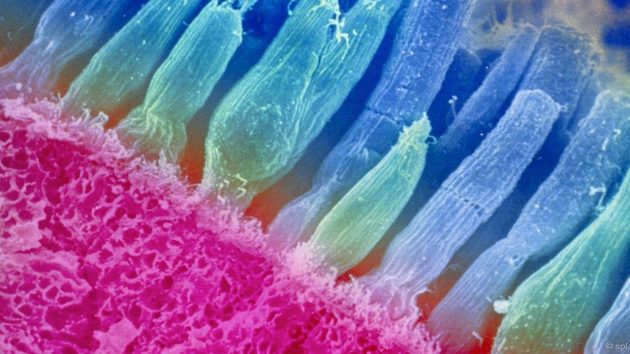
Structure of the retina
The structure of the retina is very complex. All its elements are closely connected, and damage to any of them can lead to serious consequences. The retina has a three-neuron receptor-conducting network necessary for visual perception. This network consists of photoreceptors, bipolar neurons and ganglion cells.
Layers of the retina:
- Pigment epithelium and Bruch's membrane . They perform barrier, transport, and trophic functions, prevent the penetration of light radiation, and phagocytose (absorb) segments of rods and cones. In some diseases, hard or soft drusen form in this layer - small yellow-white spots .
- Photosensory layer . It contains retinal receptors, which are outgrowths of photoreceptors - highly specialized neuroepithelial cells. Each photoreceptor contains a visual pigment that absorbs light waves of a specific wavelength. Rods contain rhodopsin, cones contain iodopsin.
- External limiting membrane . Formed by terminal plates and flat adhesive contacts of photoreceptors. The external processes of Müller cells are also localized here. The latter perform a light-conducting function - they collect light on the front surface of the retina and conduct it to the photoreceptors.
- Outer nuclear layer . It contains the photoreceptors themselves, namely their bodies and nuclei. Their outer processes (dendrites) are directed towards the pigment epithelium, and the inner ones - towards the outer reticular layer, where they contact bipolar cells.
- Outer mesh layer . Formed by intercellular contacts (synapses) between photoreceptors, bipolar cells and associative neurons of the retina.
- Inner nuclear layer . The bodies of Müllerian, bipolar, amacrine and horizontal cells lie here. The former are neuroglial cells and are necessary for maintaining nerve tissue. All others process signals coming from photoreceptors.
- Inner mesh layer . Contains internal processes (axons) of various nerve cells of the retina.
- Ganglion cells receive impulses from photoreceptors through bipolar neurons, and then conduct them to the optic nerve. These nerve cells are not covered with myelin, making them completely transparent and easily transmit light.
- Nerve fibers . They are axons of ganglion cells that transmit information directly to the optic nerve.
- Internal limiting membrane . Separates the retina of the eye from the vitreous body.
Slightly medial (closer to the middle) and upward from the center of the retina in the fundus of the eye is the optic disc. It has a diameter of 1.5-2 mm, pink color, and in its center a physiological excavation is noticeable - a small notch. In the area of the optic disc there is a blind spot, devoid of photoreceptors and insensitive to light. When determining the visual field, it is determined in the form of a physiological scotoma - loss of part of the visual field.
In the central part of the optic nerve head there is a small depression through which the central artery and vein of the retina pass. The vessels of the retina lie in the layer of nerve fibers.
Approximately 3 mm lateral (closer to the outside) of the optic disc there is a macula macula. In its center is the fovea centralis, the location of the largest number of cones. It is she who is responsible for high visual acuity. Retinal pathology in this area has the most adverse consequences.
Methods for diagnosing diseases
The standard diagnostic program includes measuring intraocular pressure, checking visual acuity, determining refraction, measuring visual fields (perimetry, campimetry), biomicroscopy, direct and indirect ophthalmoscopy.
Diagnostics may include the following methods:
- study of contrast sensitivity, color perception, color thresholds;
- electrophysiological diagnostic methods (optical coherence tomography);
- fluorescein angiography of the retina – allows you to assess the condition of the vessels;
- Fundus photography is necessary for subsequent observation and comparison.
Symptoms of retinal diseases
Most characteristic feature retinal lesions are a decrease in acuity or narrowing of visual fields. The appearance of absolute or relative scotomas of different localization is also possible. A photoreceptor defect may indicate various shapes color blindness and night blindness.
A pronounced deterioration in central vision indicates damage to the macular region, peripheral vision - to the periphery of the fundus. The appearance of a scotoma indicates local damage to a certain area of the retina. An increase in the size of the blind spot, along with a strong decrease in visual acuity, may indicate pathology of the optic nerve.
Central retinal artery occlusion results in sudden and sudden (within seconds) blindness in one eye. With ruptures and detachments of the retina, light flashes, lightning, and glare may appear in front of the eyes. The patient may complain of fog, black or colored spots in the field of vision.
Retinal diseases
According to etiology and pathogenesis, all retinal diseases are divided into several large groups:
- vascular disorders;
- inflammatory;
- dystrophic lesions;
- injuries;
- benign and malignant neoplasms.
The treatment of each retinal disease has its own characteristics.
To combat pathological changes in the retina, the following can be used:
- anticoagulants - Heparin, Fraxiparin;
- retinoprotectors - Emoxipin;
- angioprotectors - Ditsinon, Troxevasin;
- vasodilators - Sermion, Cavinton;
- B vitamins, nicotinic acid.
The drugs are administered parabulbarly (eye injections); eye drops are used less frequently. For ruptures, detachments, and severe retinopathy, laser coagulation, cerclage, episcleral filling, and cryopexy can be performed.
Inflammatory diseases are retinitis of various etiologies. Inflammation of the retina develops due to microbes entering it. If everything is simple here, then other groups of diseases should be described in more detail.
Vascular pathology
One of the most common vascular diseases retina is damage to vessels of different sizes. The cause of its development may be hypertension, diabetes mellitus, atherosclerosis, trauma, vasculitis, osteochondrosis cervical spine spine.
Initially, patients may experience dystonia or vasospasm of the retina, later hypertrophy, fibrosis or thinning of the vessels develops. This leads to retinal ischemia, which causes the patient to develop angioretinopathy. In persons with hypertension arteriovenous crossover appears, symptoms of copper and silver wire appear. Diabetic retinopathy is characterized by intense neovascularization - pathological proliferation of blood vessels.
Retinal angiodystonia is manifested by decreased visual acuity, flickering of spots before the eyes and visual fatigue. Arteriospasm can occur with increased or decreased blood pressure, some neurological disorders. In parallel with damage to arterial vessels, the patient may develop phlebopathy.
A common vascular pathology is central retinal artery occlusion (CRAO). The disease is characterized by blockage of this vessel or one of its branches, leading to severe ischemia. Central artery embolism most often occurs in individuals with atherosclerosis, hypertension, arrhythmia, neurocirculatory dystonia and some other diseases. Treatment of pathology should begin as early as possible. If medical care is not provided promptly, occlusion of the central retinal artery can lead to complete loss of vision.
Dystrophies, injuries, developmental defects
One of the most common malformations is coloboma - the absence of part of the retina. Often there are macular (mainly in older people), central, peripheral. The latter are divided into different types: ethmoid, small cystic, frost-like, “snail trail”, “cobblestone”. With these diseases, defects resembling holes of different sizes can be seen in the fundus of the eye. Pigmentary degeneration of the retina also occurs (its cause is redistribution of pigment).
After blunt trauma and contusions, Prussian opacities often appear on the retina. Treatment of the pathology consists of the use of antihypoxants, vitamin complexes. Hyperbaric oxygen therapy sessions are often prescribed. Unfortunately, treatment does not always have the expected effect.
Neoplasms
A retinal tumor is a relatively common ophthalmological pathology – it accounts for 1/3 of all neoplasms of the eyeball. Patients are usually diagnosed with retinoblastoma. Nevus, angioma, astrocytic hamartoma and other benign neoplasms are less common. Angiomatosis is most often combined with various malformations. Treatment tactics for tumors are determined on an individual basis.
The retina is the peripheral part of the visual analyzer. It carries out photoreception - the perception of light waves of different lengths, their transformation into a nerve impulse and its conduction to the optic nerve. With lesions of the retina, people experience a wide variety of visual disorders. Most dangerous consequence retinal damage causes blindness.
