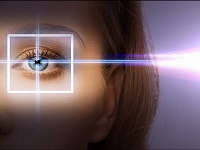
Laser treatment of cataracts.
Cataract Extraction (extractio cataractae)
surgery: removal of the lens for cataracts. Cataract extraction intracapsular(e. cataractae intracapsularis) - E. to., in which they are removed along with the capsule without opening it. Combined cataract extraction(e. cataractae combinata) - E. to., produced in combination with a complete iridectomy. Extraction of a cataract with a round pupil - E. to., made in combination with a peripheral iridectomy with preservation of a round pupil. Extracapsular cataract extraction(e. cataractae extracapsularis) - E. to., in which the lens capsule is opened and only its front part is removed.
1. Small medical encyclopedia. - M.: Medical Encyclopedia. 1991-96 2. First health care. - M.: Great Russian Encyclopedia. 1994 3. Encyclopedic Dictionary medical terms. - M.: Soviet Encyclopedia. - 1982-1984.
See what "Cataract Extraction" is in other dictionaries:
- (extractio cataractae) surgery: removal of the lens in cataracts ... Big Medical Dictionary
- (e. cataractae intracapsularis) E. to., in which the lens is removed along with the capsule without opening it ... Big Medical Dictionary
- (e. cataractae combinata) E. to., produced in combination with a complete iridectomy ... Big Medical Dictionary
E. to., produced in combination with peripheral iridectomy with preservation of the round pupil ... Big Medical Dictionary
- (e. cataractae extracapsularis) E. to., in which the lens capsule is opened and only its front part is removed ... Big Medical Dictionary
- (cryoextractio cataractae; cryo + extraction; synonym cryophakia) a method of intracapsular cataract extraction, based on freezing the tip of a special instrument to the anterior surface of the lens, followed by its extraction ... Big Medical Dictionary
CATARACT- honey. Cataract - partial or complete clouding of the substance or capsule of the lens, leading to a decrease in visual acuity up to its complete loss. Frequency Senile cataract is more than 90% of all cases 52 62 years 5% of people 75 85 years ... ... Disease Handbook
VASCULAR- eyes (chorioidea), represents the posterior portion of the vascular tract and is located posteriorly from the serrated edge of the retina (ora serrata) to the opening of the optic nerve (Fig. 1). This section of the vascular tract is the largest and embraces ... ... Big Medical Encyclopedia
It happens that during routine examinations they reveal early signs cataracts, although the patients themselves have not yet noticed any of its symptoms. It often happens that patients themselves notice the deterioration of vision caused by cataracts - this usually occurs over the age of 40 years. In most of these cases, doctors recommend that patients undergo regular examinations, and cataract surgery may not be scheduled until many years after the first symptoms appear.
When to have cataract surgery
Previous refractive surgery, such as laser vision correction Laser vision correction - which method is the most effective? . is not a contraindication to cataract removal.
cataract surgery
Cataract removal is the most common type of eye surgery. Thanks to modern development micro incision surgery, cataract surgery are carried out quickly, efficiently and with minimal subsequent pain.
Cataract Extraction
Cataract extraction is the most old way surgical removal of cataracts. This operation requires a full-fledged hospital of the patient, it is performed under general anesthesia. The operation consists in making a large incision on the cornea of the eye, from 10 to 12 millimeters long, through which the natural affected cloudy lens is removed with surgical instruments. After cleaning the lens attachment site, piece supports are installed on which the artificial lens is fixed. After the operation, sutures are applied to the eye, which are removed by the attending physician after 4-6 months.
Since a really large incision is made in the eye during cataract extraction, the postoperative rehabilitation period takes at least two months. During rehabilitation after cataract extraction, the patient very often feels pain, discomfort and visual fatigue.
In the modern world, there are two modifications of cataract extraction:
- intracapsular cataract extraction; extracapsular cataract extraction.
Intracapsular cataract extraction is performed using a special tool - a cryoextractor. This device has a special tip, which at the right time can freeze sharply to a sufficiently low temperature. The cryoextractor, through the incision of the cornea, is brought directly to the lens, after which it freezes it to itself. Such an operation is the least effective, since it injures the eye very much and, at the same time, does not completely eliminate all the affected cells of the natural lens epithelium.
Extracapsular cataract extraction is performed using a high-precision cutting instrument, due to which the lens is removed, but at the same time its posterior capsule is preserved, which is not damaged by the cataract. The safety of the posterior capsule leaves a full-fledged barrier between the posterior and anterior parts of the eye, and also accelerates the process of complete healing of the eye after surgery.
Although cataract extraction is effective way surgical elimination of the disease, due to the great trauma of the process, it has recently been used very rarely. More effective and painless ways to eliminate cataracts are laser removal and phacoemulsification.
Laser cataract removal
For the first time, the method of eliminating cataracts using a laser beam was tried more than twenty years ago, but at that time it turned out to be insufficiently effective and, at the same time, very expensive. In the modern world, laser cataract removal is the most painless way to eliminate the disease.
Phacoemulsification of cataracts
Cataract phacoemulsification is a surgery that uses an ultrasonic device to break up and remove the clouding of the lens or cataract from the eye to improve vision. Immediately after cataract phacoemulsification, an artificial lens (intraocular lens - IOL) is inserted into the eye.
Continued below ⇓
Heredity may also play a role in a person's predisposition to cataracts in more early age, the phenomenon of "advance" of presenile cataract. Cataracts can also develop as a result of trauma and physical damage to the lens. Atopy or allergy is known to hasten progression.
Purpose of cataract phacoemulsification
Cataract phacoemulsification, or phaco as it is called by surgeons, is used to restore vision that has been blurred due to cataracts in patients. On the initial stages disease, people can only notice a slight turbidity, tk. she cataract affects only a small part of the lens, the organ that focuses light on the retina. As the cataract grows, more and more light is blocked and vision becomes blurred. With vision deterioration, the surgeon recommends cataract surgery, usually phacoemulsification, to restore clear vision. With advances in cataract surgery, such as the IOL, patients can sometimes see significant improvements in vision.
Epidemiology of the disease
The likelihood of cataract formation increases with age. National Institute US Eyes (NIH) reported in a 2002 study that more than half of US residents aged 65 years and older suffer from cataracts. People who smoke have a higher risk of developing cataracts. Increased sun exposure without wearing safety glasses can also cause cataracts.
Cataracts can also occur at any time due to injury, exposure to toxins, or diseases such as diabetes. Congenital cataracts are caused by genetic defects, developmental problems, or exposure to certain infectious diseases during pregnancy.
However, the most common form of cataract in the US is related to age. According to the NIH, cataracts are more common among women than men, and Caucasians are more likely to develop cataracts, especially with age. People living closer to the equator are also at high risk due to increased sun exposure.
In the US, more than 1.5 million cataract surgeries are performed each year. The NIG reports that the US federal government spends more than $3.4 billion annually on cataract treatment through Medicare, the national social insurance company. Cataract surgery is one of the most frequently performed procedures, as well as one of the safest and most effective surgeries. Cataract phacoemulsification is currently the most popular option for cataract surgery.
Description of cataract phacoemulsification
Phacoemulsification is a type of extracapsular cataract removal, a procedure in which the lens and the front of the capsule are removed. The most popular form of cataract surgery in the past, the older extracapsular cataract surgery involves a longer incision, about 10 mm, or nearly half the eye. The recovery process after extracapsular removal with a larger incision also requires almost a week's stay in the hospital after surgery and limitation of physical activity for several weeks or even months.
Charles Kelman created cataract phacoemulsification in the late 1960s. His goal was to remove the cataract with a smaller incision, less pain, and a shorter recovery period. He discovered that cataracts could be broken up or emulsified into small pieces using an ultrasound probe. In the beginning, phacoemulsification slowly gained popularity due to its high learning curve. Surgeons have been slow to learn this technique despite its success rate and shorter recovery time. Over the decades, surgeons have continually improved cataract phacoemulsification to make it safer and more successful. Innovations in technology, such as the foldable IOL, have helped improve outcomes by allowing surgeons to make smaller incisions.
During the operation, the patient may need to breathe through an oxygen tube because breathing may be difficult due to covering with a tissue. Most likely, the medical staff will also monitor the patient's blood pressure and heartbeat.
Before making an incision, the surgeon inserts a long needle, usually through the lower eyelid, to numb the area behind the eyeball. The surgeon then applies pressure to the eyeball with a hand or weight to check for bleeding (possibly caused by an anesthetic). The pressure will stop this bleeding. This effort will also lower intraocular pressure, which will reduce the chances of complications.
After applying pressure, the surgeon will look through a microscope and make an incision about 3 mm in size from the side of the numb cornea. Since 2003, surgeons have preferred the temporal incision location because it is safer. The location of the incision also varies depending on the size and density of the cataract. After the incision is made, a viscoelastic fluid is injected to reduce intraocular tissue shock. The surgeon then makes a microscopic circular incision in the membrane that surrounds the cataract; this part of the procedure is called capsulorhexis. After that, a jet of water frees the cataract from the outer cover. The surgeon inserts a small titanium needle, or phacoemulsification probe, into the cornea. The ultrasonic waves from the phacoemulsification probe emulsify the cataract so that it can be removed by suction. First, the surgeon focuses on the denser central nucleus of the cataract.
While the cataract is being emulsified, the machine simultaneously aspirates the cataract through a small hole in the tip of the phacoemulsification probe. The surgeon then removes the outer covering of the lens, but leaves the posterior capsule, which is used to support the intraocular lens.
The injector inserts a collapsible IOL that does not require a large incision. After the introduction of the IOL into the capsular bag, the viscoelastic fluid is removed. After surgery, sutures are usually not required. Some surgeons may recommend that patients wear goggles immediately after surgery.
The whole procedure takes about 20 minutes. Cataract phacoemulsification itself only takes a few minutes.
Most surgeons prefer a certain technique for the procedure, although these may vary depending on the density and size of the cataract. Varieties of cataract phacoemulsification usually differ in which part of the nucleus the surgeon focuses on first, and how the cataract is emulsified. Some surgeons prefer a continuous "fracture" of the cataract, while others divide the cataract into quadrants for removal. In one procedure, called "supracapsular luxation of the nucleus", the surgeon inverts and then rotates the lens for removal. Improvements in technology may also allow even smaller incisions, as small as 1.4 mm.
Diagnosis/Preparation
Cataracts can take years to develop before vision is sufficiently impaired to require surgery. An optometrist may initially advise wearing glasses to temporarily improve vision. But vision will deteriorate as the lens becomes clouded.
When a cataract develops and gets worse, patients may experience the following symptoms:
- gradual (and painless) blurring of vision;
- poor central vision;
- frequent changes in corrective lens prescriptions;
- more and more glare in the eyes from the light;
- improving near vision to the point where reading glasses are not needed;
- blurred vision in the sun.
Cataracts develop faster in younger people and diabetics, so in such cases, doctors recommend surgery as soon as possible. The doctor may also recommend surgery as soon as possible if the patient suffers from other eye diseases, such as age-related degeneration macula, and if the cataract interferes with a complete examination of the eye.
If symptoms worsen to the point where daily activities become problematic, surgery is necessary. A complete eye examination will determine the severity of the cataract and the type of surgery that will be performed on the patient. For denser types of cataracts, the old method of extracapsular removal is preferred.
The diagnostic examination should include measurement of low and high light visual acuity, microscopic examination of ocular structure and pupillary dilation, assessment of the visual field, and measurement of intraocular pressure (IOP).
If cataracts are found in both eyes, each eye should be treated separately.
It is also necessary to take into account general health patient and how it will affect the outcome of the operation. Before the operation, the surgeon may recommend a general physical examination.
Although preoperative instructions may vary, patients are usually asked not to eat or drink anything after midnight on the day of surgery. All medications taken should be reported to determine if they need to be discontinued prior to surgery. Patients taking aspirin to thin their blood are usually asked to stop taking it two weeks before surgery. Blood-thinning drugs can increase the risk of intraocular bleeding or hemorrhage. Coumadin, a blood thinner, should be taken if the patient is at high risk of a seizure. To determine the course of action, you need to consult with your optometrist and therapist.
To determine the length eyeball an A-scan will be performed. This helps determine the refractive power of the IOL. Other pre-operative tests such as x-rays may be required chest, blood or urine test if there are other medical problems.
The surgeon may also require the patient to start using antibiotic drops before surgery to limit the possibility of infection.
Cataract surgery is performed on an outpatient basis, so the patient needs to arrange for someone to be taken home after the operation. On the day of the operation, the doctor will review the preoperative tests again and introduce expanding eye drops, antibiotic drops, corticosteroid or non-steroidal anti-inflammatory drops. Anesthetic eye drops will be administered to both eyes for convenience during the operation. A local anesthetic is also injected. The patient remains conscious during the operation, but remains relaxed.
Before the operation, the patient's eye is washed, and his shoulders and head are covered with a sterile napkin. The patient is required to lie still and focus on the light of the operating microscope. A dilator is inserted into the eye to prevent the eyelids from closing.
Care after cataract phacoemulsification
Immediately after cataract surgery, the patient is examined in an outpatient recovery room. The patient is advised to rest for at least 24 hours before returning to the doctor's office for a checkup. On the day of surgery, only light meals are recommended. The patient may still feel drowsy, as well as experience pain in the eye or discomfort. Over-the-counter drugs are usually recommended for pain relief, but the patient should check with their doctor if they are needed. The surgeon should be informed immediately of any other side effects such as severe pain, nausea, or vomiting.
During the recovery period, some changes will occur in the eye. The patient may see dark spots, which should disappear within a few weeks after the operation. There may also be discharge from the eye and itching. A warm, moist compress can be applied for 15 minutes to relieve itching and discharge, which should be gently cleaned with a cloth, not with your finger. You may also experience pain and sensitivity to light after surgery. In some patients, the skin of the eyes may droop slightly, or there may be bruising that disappears as it heals.
The first postoperative visit to the doctor takes place the day after the operation. The surgeon will remove goggles and prescribe eye drops to prevent infections and control intraocular pressure. These eye drops are used for about a month after surgery.
The patient is advised to wear goggles while sleeping and not rub their eyes for at least two weeks. During this period, the doctor will give the patient special colored sunglasses or ask him to wear regular prescription glasses to prevent possible injury to the eye from accidental friction or impact. Unlike other types of cataract surgery, patients after cataract phacoemulsification can immediately resume their normal activities.
Follow-up visits are usually weekly, every three weeks, and every six to eight weeks after surgery. However, this may vary depending on any complications or any unusual postoperative symptoms.
After the healing process, the patient may need new corrective lenses, at least for near vision. Although the IOL can be removed due to the need for myopic correction, the patient may need new lenses for near work.
Operation risks
The likelihood of complications is low, but they can occur. Patients may experience unexpected bleeding from the wound and re-inflammation after surgery. A few weeks after surgery, flashes, flies in the eyes, and double vision may occur. These symptoms should be reported to the surgeon immediately. Some can be easily treated, while others, such as flies, can be a sign of a retinal detachment.
Retinal detachment is one of the possible serious complications. The retina can detach due to surgery if there was retinal weakness during the surgery. This complication may not occur for weeks or months.
Infections are another complication, the most serious being endophthalmitis, an infection of the eyeball. This complication, which was often reported in the past, is now not too common thanks to new surgical techniques and antibiotics.
Patient anxiety can also be caused by IOL misalignment, but newer IOL designs limit the possibility of IOL misalignment.
Other possible complications are the development of glaucoma and, in very rare cases, blindness.
There is a possibility of developing a secondary cataract in the remaining posterior part of the capsule. This may occur up to two years after the operation. Laser-assisted AIH capsulotomy is most commonly used to remove secondary cataracts. This outpatient procedure does not require an incision. The laser makes a small hole in the remaining back of the lens to allow light to enter.
Normal results
In most cases, patients restore visual activity after surgery, and some begin to see best after the introduction of the IOL. Some patients no longer need to wear glasses after cataract surgery. contact lenses. Patients have improved color and depth perception and can continue normal activities that had to be stopped due to visual impairment from cataracts (driving, reading, or playing sports).
Morbidity and mortality rates
Cataract phacoemulsification took into account the risks of previous cataract surgeries, making it a safer procedure. Before phacoemulsification, death from cataract surgery was uncommon, but it usually occurred from possible complications due to general anesthesia. Cataract phacoemulsification is performed under local anesthesia, limiting the risks of general anesthesia.
Other serious complications such as blindness also became less frequent with widespread phacoemulsification of cataracts. Improved antibiotics have allowed physicians to fight the old debilitating infections that caused blindness.
Alternatives
If the cataract is too large to be removed through a small incision, older methods of cataract surgery may be needed, including:
- Extracapsular cataract removal. Although cataract phacoemulsification is considered a type of extracapsular removal, an older version of this technique requires a much larger incision and does not use a phacoemulsification machine. The procedures are similar in that the lens and anterior part of the capsule are removed and rear part the capsule remains. The surgeon may consider using this technique if the patient has corneal disease or the pupil is too small during the first phase of the operation.
- Intracapsular cataract removal. It also requires a larger incision than in cataract phacoemulsification. The method differs in that both the lens and the entire capsule are removed. While this operation is considered the most technically simple for the surgeon, this method increases the risk of retinal detachment and swelling after the operation. The recovery period is longer and in most cases patients have to wear large "cataract glasses" to see.
Learn more about cataracts:
Cataract - treatment and surgery, symptoms and signs
Cataract treatment and removal surgery
Cataract surgery - price
Modern medicine recognizes the only effective method cataract treatment, and this is a surgical operation to remove it.
Types of cataract surgery
- Cataract removal with lens replacement is the main type of ophthalmic surgery performed today. There are two types of cataract extraction and phacoemulsification.
- Intracapsular cataract extraction - removal of the lens capsule together with the capsule through a large incision in the cornea.
- Extracapsular cataract extraction - removal of the clouded lens while maintaining the posterior capsule.
Cataract surgery: price
Modern methods of conducting surgical intervention for the purpose of cataract removal provide high efficiency and maximum safety of the process. Like any surgical operation, laser and other removal of the clouded lens may have some contraindications and limitations. Therefore, before surrendering to the hands of surgeons, it is necessary to conduct a comprehensive examination of the body, to pass tests. Preliminary diagnostic procedures allow you to identify refractive disorders, make sure that there are no contraindications for surgery and prescribe the most appropriate type of intervention.
When cataract surgery is performed, the price for it is determined individually for each patient, as different types pre- and postoperative procedures and analyses. A separate vision correction scheme is developed for each patient. price for each separate view services in commercial clinics can be found on the websites medical centers. The final price for a full package of services can be found after consultation in the clinics themselves.
Approximate prices for cataract surgery
- Cataract removal in the presence of lens subluxation with IOL suturing - about 35 thousand rubles.
- Cataract phacoemulsification with implantation of a flexible IOL - about 35-40 thousand rubles.
- Cataract phacoemulsification with lens replacement for a soft aspherical IOL - 42-45 thousand rubles. rub.
- Phacoemulsification of a cataract and implantation of a multifocal IOL - approximately 98-115 thousand rubles.
- Phacoemulsification with IOL implantation, plus antiglaucoma surgery - 59 thousand rubles.
To the price of the operation, the amount for a certain type of procedure that is necessary in a particular case can also be added.
Cataract surgery - phacoemulsification
The only effective, reliable, painless and modern method cataract removal - phacoemulsification with implantation of an artificial intraocular lens. Excimer clinic specialists offer this kind of operation to their patients.
For cataract surgery, it is not necessary, as before, to wait until the cataract "ripens" and endure a gradual decrease in vision. The process of "ripening" of a cataract can take up to 10 years or more, so earlier a person sometimes had to leave his job because of this disease, he could no longer drive a car, he experienced inconvenience in low light, his whole habitual way of life was disrupted. Now cataract removal is possible on the most early stages disease development.
Illustration of the progress of the operation
Stages of cataract surgery using ultrasonic phacoemulsification:
Using a diamond instrument, the ophthalmic surgeon creates a micro-incision of 2.5 mm in size. and all further manipulations during the operation are carried out through it;
Viscoelastic is introduced into the anterior chamber of the eye using a cannula - a special substance that protects the internal structures of the eye during the operation from ultrasonic and mechanical effects and allows the ophthalmic surgeon to freely perform all the necessary manipulations;
The ophthalmic surgeon inserts a special probe through a micro-incision, which, with the help of ultrasound, makes it possible to turn the lens affected by the cataract into an emulsion;
Through a micro-incision, a flexible intraocular lens is inserted into the capsule, where the lens was previously located, in a folded state, which independently unfolds inside the eye and is securely fixed. Now the intraocular lens will perform the functions of the lens;
At the end of the operation, the entire mass of viscoelastic is washed out of the anterior chamber of the eye using an irrigation solution.
Modern ophthalmosurgery of small incisions allows cataract phacoemulsification without subsequent suturing, since the microincision is self-sealing. This makes it possible in the future not to limit physical and visual stress. The patient begins to see well immediately after the operation, and the maximum visual acuity is restored within a period of two days to a week. In Excimer clinics, cataract surgery is performed on a one-day basis, without hospitalization. This is a complex microsurgical intervention, but all its stages are provided by the use of modern techniques and materials.
Cataract surgery is recognized by the World Health Organization as the only completely rehabilitative operation among all, and not only eye, surgical interventions.
To make an appointment
When registering through the site, a 5% discount on vision diagnostics
What is the best surgical technique for lens opacity - laser cataract treatment or extracapsular cataract extraction? Of course, today laser methods of treatment are more popular. They are less traumatic, after the operation there are no complications. The only drawback is the cost of the operation. For many people, it is simply not available.
Standard strip surgery is much cheaper than laser surgery. But, if all the recommendations of the doctor are followed, the person adheres to the rules of the rehabilitation period, complications can also be avoided, as in the case of laser surgery.
Extracapsular cataract extraction is a classic operation that is used to remove the lens of the eye. Today, the method remains relevant and is performed by many well-known clinics.
It is a cavity operation.
- Before surgery begins, patients undergo a complete diagnosis: they pass tests.
- If necessary, doctors may order an ultrasound.
- On the day when the extracapsular extraction is performed, the patient's blood pressure will be measured and a special agent will be introduced that will dilate the pupil.
- The operation is performed under local anesthesia. If a person is nervous and worried, doctors may decide to give the patient a sedative.
- The incision is made with a sharp diamond knife. The cloudy and cataract-affected lens is removed from the eye cavity. The doctor then inserts the implant. After that, the incision is sutured, an aseptic bandage is applied.
- To exclude the possibility of complications, anti-inflammatory drugs and antibiotics are prescribed during the rehabilitation period.
Cataract extraction, in which the lens is removed, is considered a traumatic technique, because a large incision is made and stitches are applied to the postoperative wound.
Despite the fact that this technique is very popular, it is intensively replaced by ultramodern low-traumatic methods. surgical treatment. One of them is femtolaser surgery, which involves the removal of the lens.
Femtolaser technique
Femtolaser cataract surgery is the pinnacle of ophthalmic surgery. The operation is performed using a robotic technique equipped with a laser.
Laser pulses are focused to a clearly defined depth, while crushing the lens is ensured. In addition, laser systems are fully automatic. This greatly simplifies the work of the doctor who performs the operation. The duration of the operation is reduced, the safety of the patient is ensured.
All the procedures that the doctor performs during extracapsular extraction, with laser treatment made by robotics. That is, the laser itself dissects the shell of the eye, opens the anterior capsule of the lens, and crushes it.
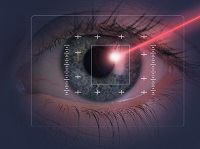
The main feature of the operation is that the clouded lens is destroyed without opening it. Another advantage is that the laser is not able to damage the cornea.
The main advantages of laser eye treatment:
- High accuracy of surgical intervention. Ultra-precise performance of the procedure by robotic technology allows you not to affect healthy eye tissue.
- Fast recovery period. No mechanical instruments are used for the eyes. All punctures that will be made in the eye area quickly coagulate.
- Laser is a gentle operation. This minimizes the impact of ultrasonic waves on the internal structure of the eye. As a result, there is no risk of corneal edema after surgery.
- Significantly improved visual performance. Thanks to the precision of laser equipment, doctors achieve maximum visual acuity and quality.
- Vision is restored within 2-3 hours.
- The stability of the general condition of the patient after removal of the lens. High-tech equipment used during surgical laser intervention makes it possible to accurately predict the result.
When is the best time to have the operation?
It is better to remove the lens immediately after a person has noticed a deterioration in vision.
Important! It is impossible to get rid of such a disease as - it is impossible. And this should be well learned by people who have already been diagnosed with the disease.
Neither a drop, nor a pill, nor the most effective Tibetan and folk methods will help get rid of the clouding of the lens. This process is irreversible!
With recipes traditional medicine And medicines You can only extend the period of remission, but no more. After a while, the person will again feel a deterioration in vision. We must not forget that they can be the most unpredictable.
When, the risk of complications develops. In the late stage, the lens increases in volume. In some cases, its thickness breaks through the shell into the inner region of the eye. At the same time, the outflow tracts of intraocular fluid are squeezed and clogged.

The result is the development of secondary glaucoma, complete loss of vision. This process is irreversible, and it is impossible to restore vision in the future.
Therefore, doctors strongly recommend not to treat with medications even in the initial stages, but to immediately replace the affected lens. In no case should you self-medicate, especially folk remedies. People come up with such tales, from which doctors traditional medicine"The hair stands on end."
It should be remembered that in no case should you make lotions from improvised means that contain aggressive chemical substances. For example, some resources carry information that laundry soap can help cure eye cataracts, but this is nonsense and nothing more. Most best option to remain a sighted person, to get rid of cataracts forever - this is an operation.
Which method of removal a person chooses depends only on his material capabilities and desires. Of course, it is better to give preference to laser therapy.
For many years, the corneal surgical incision for extracapsular cataract extraction has been the method of choice in many clinics around the world. The operation begins with the formation of an operating incision, which is carried out along the front edge of the surgical limbus with a pointed diamond knife to a depth of 650 microns at a distance of 1.5 mm from the limbus in the meridian from 10 to 14 hours. Then paracentesis is performed for 12 or 14 hours. Next, an endothelial protector is inserted and the anterior capsule is dissected with Fedorov's cystotome by applying multiple microperforations along the chord connecting the ten and two o'clock segments. "Cutting" of the deep layers of the cornea is carried out with a blunt diamond knife of the "Sokha" type. In this case, the lower platform of the knife slides along the anterior surface of the root zone of the iris without damaging it.
Removal of the lens nucleus is the central and crucial stage extracapsular cataract extraction. Its implementation can be associated with certain difficulties and complications. The widespread introduction of viscoprotectors, the use of "endocapsular" technology contributed to a decrease in trauma during the removal of the nucleus. After careful hydrodissection with a spatula, lightly press on the scleral lip of the surgical incision in the meridian of 12 hours. This exposes and lifts the upper pole of the lens. Then, with a Sato knife or a second spatula, the lens nucleus is removed from the anterior chamber. At the same time, the anterior capsule and the previously introduced viscoelastic protect the posterior surface of the cornea from damage.
The evacuation of the lens masses is carried out using a Simcoe cannula or a dual-channel aspiration-irrigation cannula connected to a syringe. The elasticity of the cannula, the presence of a ball at its working end eliminate the risk of capturing the lens capsule during aspiration, and allow mechanical separation of the lens fibers from the posterior lens capsule.
