What applies to glandular organs? Glandular epithelia
LECTURE No. 5
Age-related endocrinology
Plan.
Classification of glands of the human body.
Characteristics of hormones.
Particular characteristics of the endocrine glands, their age characteristics.
All glands of the human body are divided into three groups.
Glands external secretion or exocrine have excretory ducts through which the substances formed in them are excreted into various cavities or on surface bodies. This group includes the liver, salivary, lacrimal, sweat, and sebaceous glands.
Glands internal secretion or endocrine do not have excretory ducts, the substances they synthesize - hormones - enter directly into the blood. This group includes the pituitary gland, pineal gland, thyroid and parathyroid glands, thymus, and adrenal glands.
Glands mixed secretions have both exocrine and intrasecretory functions. These are the pancreas and gonads.
Hormones- these are physiologically active substances that participate along with nervous system in the regulation of almost all processes occurring in the body. They regulate metabolism (protein, fat, carbohydrate, mineral, water), helping to maintain homeostasis. Hormones influence the growth and formation of organs, organ systems and the entire body as a whole. Under the influence of hormones, tissue differentiation occurs; they can have a triggering effect on the effector organ or change the intensity of functioning of various organs. Hormones regulate biological rhythms and ensure adaptive reactions of the body under the influence of stress factors.
Hormones have:
high biological activity, i.e. hormones have an effect in very small concentrations;
specificity of action, i.e. hormones affect only target cells and target organs; phenomena that occur due to insufficiency of one of the glands can disappear only when treated with hormones of the same gland;
distance of action, i.e. hormones can act on certain organs located at a great distance from the place of their release)
Human endocrine glands are small in size, have a small mass (from fractions of a gram to several grams), and are richly supplied with blood vessels. Blood brings the necessary building material to them and carries away chemically active secretions. The activity of the endocrine glands changes significantly under the influence of pathological processes. It is possible either to increase the secretion of hormones - hyperfunction glands, or decrease - hypofunction glands. Disturbances in the functioning of the endocrine glands in children have more negative consequences than in adults. However, as children and adolescents grow and develop, normal hormonal imbalances may occur, such as during puberty.
Particular characteristics of the endocrine glands.
Thyroid gland a newborn weighs about 1 g, at 5–10 years its weight increases to 10 g. Particularly intensive growth thyroid gland observed at 11–15 years of age, during this period its weight is 25–35 g, i.e. almost reaches the level of an adult.
The thyroid gland secretes thyroid hormones thyroxine and triiodothyronine, which contain iodine. These hormones stimulate growth and development in the intrauterine period of ontogenesis. They are especially important for the full development and functioning of the nervous and immune systems. Under the influence of these hormones, heat production increases (calorigenic effect), and the metabolism of proteins, fats and carbohydrates is activated.
The thyroid gland also produces the hormone calcitonin, which ensures the absorption of calcium by bone tissue. The role of this hormone is especially important in children and adolescents, which is associated with increased skeletal growth.
Hypofunction of the thyroid gland in childhood can lead to serious mental development disorders - from minor dementia to idiocy. These disorders are accompanied by delayed growth, physical development and puberty, decreased performance, drowsiness, and speech disorders. This disease is called cretinism. Early detection of thyroid hypofunction and adequate treatment have a positive effect
Hypofunction of the thyroid gland in adults leads to the development of myxedema, hyperfunction - to the development of Graves' disease. With a lack of iodine in food, the thyroid tissue grows, and endemic goiter occurs.
Parathyroid glands. Usually there are four of them, their total mass is only 0.1 g. Their hormone is parathyroid hormone - promotes decay bone tissue and the release of calcium into the blood, therefore, with its excess, the calcium content in the blood increases. Lack of parathyroid hormone, which sharply reduces the concentration of calcium in the blood, leads to the development of seizures, increases the excitability of the nervous system, and many disorders of autonomic functions and skeletal formation. Rarely, hyperfunction of the parathyroid glands causes skeletal decalcification (“softening” of the bones) and skeletal deformation. With increased activity of the parathyroid glands, the kidneys are affected; calcium deposition occurs in many organs, including the myocardium and heart vessels.
Adrenal glands- paired glands, consist of two dissimilar tissues - the cortex and the medulla. Hormones of the steroid structure are produced in the cortex - corticosteroids. There are three groups of corticosteroids: 1) glucocorticoids, 2) mineralocorticoids and 3) analogues of some hormonal products of the gonads.
Glucocorticoids (cortisol) have a powerful effect on metabolism. Under their influence, new formation of carbohydrates occurs from non-carbohydrates, especially protein breakdown products (hence their name). Glucocorticoids have a pronounced anti-inflammatory and antiallergic effect, and are also involved in ensuring the body's resistance under stress. Their role in children and adolescents is especially important in ensuring full adaptation to “school” stressful situations (moving to a new school, exams, tests etc.).
Mineralocorticoids (aldosterone) regulate mineral and water metabolism. With a lack of aldosterone, excess sodium loss from the body and dehydration are possible. Excess of it increases inflammatory processes.
Androgens and estrogens of the adrenal cortex are close in their action to sex hormones synthesized in the sex glands - testes and ovaries, but their activity is significantly less. However, in the period before the onset of full maturation of the testes and ovaries, androgens and estrogens play a decisive role in the hormonal regulation of sexual development.
In children under 6-8 years of age, the adrenal cortex secretes gluco- and mineralocorticoids, but produces almost no sex hormones.
The adrenal medulla produces norepinephrine And adrenalin. Adrenaline increases the heart rate, increases the excitability and conductivity of the heart muscle, narrows the small arteries of the skin and internal organs(except for the heart and brain), which increases blood pressure. It inhibits contractions of the stomach muscles and small intestine, relaxes the bronchial muscles. Adrenaline increases performance skeletal muscles while working. Under its influence, the breakdown of liver glycogen increases and hyperglycemia occurs. Norepinephrine primarily increases blood pressure.
The secretion of norepinephrine and adrenaline is very important in situations that require the mobilization of strength and emergency reactions of the body. Therefore, W. Cannon called them “fight and flight hormones.” The content of many adrenal hormones depends on the physical fitness of the child’s body. A positive correlation has been found between adrenal activity and physical development children and teenagers. Physical activity significantly increases the content of hormones that provide the body's protective functions, and thereby contributes to optimal development.
Pituitary, or the inferior medullary appendage is located in the sella turcica of the main bone, under the hypothalamus. In an adult, the pituitary gland weighs approximately 0.5 g. At birth, its weight does not exceed 0.1 g, but by the age of 10 it increases to 0.3 g and adolescence reaches adult level. The human pituitary gland is usually divided into three lobes.
In the anterior lobe of the pituitary gland somatotropin (growth hormone) and other tropic (stimulating) hormones are produced.
Somatotropin enhances protein synthesis, stimulates the breakdown of fat (lipolytic effect), which explains the decrease in fat deposits in children and adolescents during periods of increased growth.
Lack of growth hormone manifests itself in short stature (height below 130 cm), delayed sexual development; the proportions of the body are preserved. This disease is called pituitary dwarfism and is most often observed in children 5–8 years old. The mental development of pituitary dwarfs is usually not impaired.
Excess growth hormone in childhood leads to gigantism. This disease is observed relatively rarely: on average, there are 2-3 cases per 1000 people. The medical literature describes giants with a height of 2 m 83 cm and even more (3 m 20 cm). Giants are characterized by long limbs, lack of sexual function, and reduced physical endurance. Gigantism can appear at the age of 9-10 years or during puberty.
Adrenocorticotropic hormone stimulates the growth of the adrenal cortex and the biosynthesis of its hormones. The lack of ACTH secretion due to removal or destruction of the anterior pituitary gland makes it impossible for the body to adapt to stressors. It can have an effect on metabolism independently of the adrenal cortex (increases oxygen consumption, stimulates the breakdown of fat in adipose tissue), and promotes memory formation.
Thyroid-stimulating hormone controls the growth and maturation of the follicular epithelium of the thyroid gland and the main stages of the biosynthesis of thyroid hormones.
Gonadotropins control the activity of the gonads.
Regulation of the synthesis and secretion of adenohypophysis hormones is carried out by the hypothalamus.
From hormones of the intermediate lobe of the pituitary gland The most studied is melanotropin, which regulates the color of the skin. Under the influence of melanotropin, pigment grains are distributed throughout the entire volume of skin cells, as a result of which the skin of this area acquires a dark tint. The so-called pigment spots of pregnancy and increased pigmentation of the skin of old people are signs of hyperfunction of the intermediate lobe of the pituitary gland.
TO hormones of the posterior lobe of the pituitary gland include vasopressin and oxytocin. They are synthesized in the hypothalamus, and the posterior lobe of the pituitary gland serves as a kind of reserve organ for these hormones.
Vasopressin (antidiuretic hormone, or ADH) enhances the reabsorption of water from primary urine and also affects the salt composition of the blood. When the amount of ADH in the blood decreases, diabetes insipidus occurs (diabetes insipidus), in which up to 10-20 liters of urine are released per day. Together with the hormones of the adrenal cortex, ADH regulates water-salt metabolism in the body.
Oxytocin stimulates contraction of the uterine muscles and promotes expulsion of the fetus during childbirth. In addition, it increases milk production by the mammary glands as a result of contraction of the myoepithelial cells of the alveoli and mammary ducts of the mammary glands.
Pineal gland secretes melatonin, which serves as a physiological brake on the development of the gonads. Destruction of the pineal gland in children leads to premature puberty. Hyperfunction of the pineal gland causes obesity and the phenomenon of hypogenitalism. Pineal gland hormones take part in the regulation of biological rhythms.
Thymus gland ( thymus) is formed in the 6th week of intrauterine development. This is a lymphoid organ, well developed in childhood. Its greatest mass in relation to body weight is observed in both the fetus and a child under 2 years of age. After 2 years, the relative mass of the gland decreases, and the absolute mass increases and becomes maximum during puberty.
The thymus plays an important role in the immunological defense of the body, in particular in the formation of immunocompetent cells, i.e. cells capable of specifically recognizing an antigen and responding to it with an immune response. This is done with the help of thymus hormones - thymosins and thymopoietins.
In children with congenital underdevelopment of the thymus, lymphopenia occurs (a decrease in the content of lymphocytes in the blood) and the formation of immune bodies sharply decreases, which leads to frequent death from infections. Currently, thymic hormone preparations are already being used to correct immunological deficiency in humans.
Pancreas refers to mixed glands: here pancreatic juice (external secretion) is formed, which plays an important role in digestion; here, in the cells of the “islands” of the gland, the secretion of hormones takes place, taking part in the regulation of carbohydrate metabolism.
Hormone insulin reduces blood glucose levels, increasing the permeability of cell membranes to it. It increases the formation of fat from glucose and inhibits the breakdown of fat. Lack of insulin leads to the development of diabetes.
There is little data on age-related characteristics of insulin secretion in children. However, it is known that resistance to glucose load in children under 10 years of age is higher, and the absorption of dietary glucose occurs much faster than in adults. This explains why children love sweets so much and consume them in large quantities without danger to their health. With old age, this process slows down significantly, which indicates a decrease in the insular activity of the pancreas. Most often, middle-aged people, mostly over 40 years old, suffer from diabetes, although there are also frequent cases of congenital diabetes, which is associated with a hereditary predisposition. Children also suffer from this disease, most often from 6 to 12 years old, i.e. during the period of fastest growth. During this period, diabetes mellitus sometimes develops against the background of previous infectious diseases (measles, chicken pox, pig).
Glucagon promotes the breakdown of liver glycogen into glucose. Therefore, its administration or increased secretion increases the level of glucose in the blood, i.e. causes hyperglycemia. In addition, glucagon stimulates the breakdown of fat in adipose tissue.
Sex glands are also mixed. Here, both sex cells - sperm and eggs - and sex hormones are formed.
Male sex hormones are produced in the male gonads - the testes - androgens (testosterone and androsterone). Male sex hormones determine the development of the reproductive system, the growth of the genital organs, the development of secondary sexual characteristics: brittleness and deepening of the voice, changes in physique, and the pattern of hair growth on the face and body. Androgens stimulate protein synthesis in the body, which is why men tend to be larger and more muscular than women. Hyperfunction of the testes in early age leads to accelerated puberty, body growth and premature appearance of secondary sexual characteristics. Damage or removal of the testes at an early age leads to underdevelopment of the genital organs and secondary sexual characteristics, as well as a lack of sexual desire. Normally, the testes function throughout a man’s life.
Female sex hormones are produced in the female gonads - the ovaries - estrogens, which have a specific effect on the development of the genital organs, the production of eggs and their preparation for fertilization, and affect the structure of the uterus and mammary glands. Ovarian hyperfunction causes early puberty with pronounced secondary sexual characteristics and early onset of menstruation. In old age, women experience menopause, caused by the fact that all or almost all of the follicles with the eggs they contain are used up.
The process of puberty proceeds unevenly; it is usually divided into certain stages, each of which is characterized by the specific contribution of nervous and endocrine regulation.
Bezrukikh M.M. and others. Age-related physiology (Physiology of child development): Textbook. aid for students higher ped. textbook institutions/M.M.Bezrukikh, V.D.Sonkin, D.A.Farber. - M.: Publishing center "Academy", 2002. - 416 p.
Drzhevetskaya I.A. Endocrine system of a growing organism: Textbook. manual for biol. specialist. universities – M.: Higher school, 1987. – 207 p.
Ermolaev Yu.A. Age-related physiology: Proc. manual for pedagogical students. universities – M.: Higher. school, 1985. – 384 p.
Obreimova N.I., Petrukhin A.S. Fundamentals of anatomy, physiology and hygiene of children and adolescents: Textbook. aid for students defectol. fak. higher ped. textbook establishments. – M.: Publishing Center “Academy”, 2000. – 376 p.
Khripkova A.G. and others. Age-related physiology and school hygiene: A manual for pedagogical students. Institute/A.G. Khripkova, M.V. Antropova, D.A. Farber. – M.: Education, 1990. – 319 p.
These epithelia are characterized by secretory function. Glandular epithelium (epithelium glandulare) consists of glandular, or secretory, epithelial cells (glandulocytes). They carry out the synthesis, as well as the release of specific products - secretions onto the surface of the skin, mucous membranes and in the cavities of a number of internal organs (external - exocrine secretion) or into the blood and lymph (internal - endocrine secretion).
Through secretion, many important functions are performed in the body: the formation of milk, saliva, gastric and intestinal juice, bile, endo-
crine (humoral) regulation, etc. Most cells are distinguished by the presence of secretory inclusions in the cytoplasm, well-developed endoplasmic reticulum and Golgi complex, polar arrangement of organelles and secretory granules.
Secretory epithelial cells lie on the basement membrane. Their shape is very diverse and varies depending on the phase of secretion. The kernels are usually large, often irregular in shape. In the cytoplasm of cells that produce protein secretions (for example, digestive enzymes), a granular endoplasmic reticulum is well developed. In cells that synthesize non-protein secretions (lipids, steroids), an agranular endoplasmic reticulum is expressed. The Golgi complex is extensive. Its shape and location in the cell change depending on the phase of the secretory process. Mitochondria are usually numerous. They accumulate in places of greatest cell activity, i.e. where secretions are formed. The cytoplasm of cells usually contains secretory granules, the size and structure of which depend on chemical composition secret. Their number fluctuates depending on the phases of the secretory process. In the cytoplasm of some glandulocytes (for example, those involved in the formation of hydrochloric acid in the stomach), intracellular secretory tubules are found - deep invaginations of the plasmalemma, covered with microvilli. The plasmalemma has a different structure on the lateral, basal and apical surfaces of cells. At the first, it forms desmosomes and tight locking junctions. The latter surround the apical (apical) parts of the cells, thus separating the intercellular gaps from the lumen of the gland. On the basal surfaces of cells, the plasmalemma forms a small number of narrow folds that penetrate the cytoplasm. Such folds are especially well developed in the cells of glands that secrete secretions rich in salts, for example in the cells of the excretory ducts of the salivary glands. The apical surface of the cells is covered with microvilli.
Polar differentiation is clearly visible in glandular cells. It is due to the direction of secretory processes, for example, during external secretion from the basal to the apical part of the cell.
Periodic changes in the glandular cell associated with the formation, accumulation, release of secretion and its restoration for further secretion are called secretory cycle.
To form secretions from the blood and lymph, various inorganic compounds, water and low molecular weight organic substances: amino acids, monosaccharides, fatty acids etc. Sometimes larger molecules penetrate into the cell by pinocytosis organic matter, such as proteins. Secrets are synthesized from these products in the endoplasmic reticulum. They move through the endoplasmic reticulum to the Golgi complex zone, where they gradually accumulate, undergo chemical rearrangement and form into granules that are released from epithelial cells. An important role in the movement of secretory products in epithelial cells and their secretion is played by cytoskeletal elements - microtubules and microfilaments.
Rice. 6.9. Different types of secretion (diagram):
A- merocrine; b- apocrine; V- holocrine. 1 - poorly differentiated cells; 2 - degenerating cells; 3 - collapsing cells
However, the division of the secretory cycle into phases is essentially arbitrary, since they overlap each other. Thus, the synthesis of secretion and its release proceed almost continuously, but the intensity of secretion may either increase or decrease. In this case, the release of secretion (extrusion) can be different: in the form of granules or by diffusion without forming into granules or by converting the entire cytoplasm into a mass of secretion. For example, in cases of stimulation of the glandular cells of the pancreas, all secretory granules are quickly released from them, and after that, within 2 hours or more, the secretion is synthesized in the cells without forming into granules and is released diffusely.
The mechanism of secretion in different glands is not the same, and therefore three types of secretion are distinguished: merocrine (eccrine), apocrine and holocrine (Fig. 6.9). At merocrine type secretion, glandular cells completely retain their structure (for example, cells of the salivary glands). At apocrine type secretion, partial destruction of glandular cells (for example, mammary gland cells) occurs, i.e., along with secretory products, either the apical part of the cytoplasm of glandular cells (macroapocrine secretion) or the tips of microvilli (microapocrine secretion) are separated.
Holocrine type secretion is accompanied by the accumulation of secretion (fat) in the cytoplasm and the complete destruction of glandular cells (for example, cells of the sebaceous glands of the skin). Restoration of the structure of glandular cells occurs either by intracellular regeneration (with mero- and apocrine secretion), or with the help of cellular regeneration, i.e., division and differentiation of cambial cells (with holocrine secretion).
Secretion is regulated using neural and humoral mechanisms: the former act through the release of cellular calcium, and the latter primarily through the accumulation of cAMP. At the same time, enzyme systems and metabolism, the assembly of microtubules and the reduction of microfilaments involved in intracellular transport and excretion of secretions are activated in glandular cells.
Glands are organs that produce specific substances of various chemical natures and secrete them into the excretory ducts or into the blood and lymph. The secretions produced by the glands are important for the processes of digestion, growth, development, interaction with the external environment, etc. Many glands are independent, anatomically designed organs (for example, the pancreas, large salivary glands, the thyroid gland), some are only part of the organs (for example , stomach glands).
The glands are divided into two groups: endocrine glands, or endocrine, And exocrine glands, or exocrine(Fig. 6.10, a, b).
Endocrine glands produce highly active substances - hormones, entering directly into the blood. Therefore, they consist only of glandular cells and do not have excretory ducts. All of them are included in endocrine system of the body, which, together with the nervous system, performs a regulatory function (see Chapter 15).
Exocrine glands produce secrets, released into the external environment, i.e. on the surface of the skin or in the cavities of organs lined with epithelium. They can be unicellular (for example, goblet cells) or multicellular. Multicellular glands consist of two parts: secretory or terminal sections (portiones terminalae) and excretory ducts (ductus excretorii). The terminal sections are formed secretory epithelial cells, lying on the basement membrane. The excretory ducts are lined with various
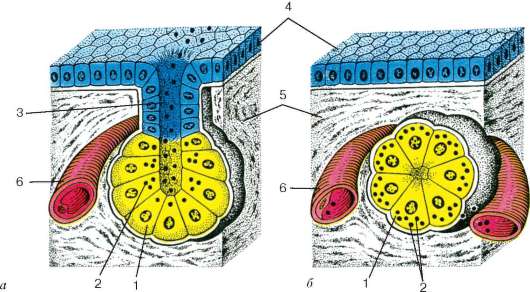
Rice. 6.10. The structure of exocrine and endocrine glands (according to E. F. Kotovsky): A- exocrine gland; b- endocrine gland. 1 - end section; 2 - secretory granules; 3 - excretory duct of the exocrine gland; 4 - covering epithelium; 5 - connective tissue; 6 - blood vessel
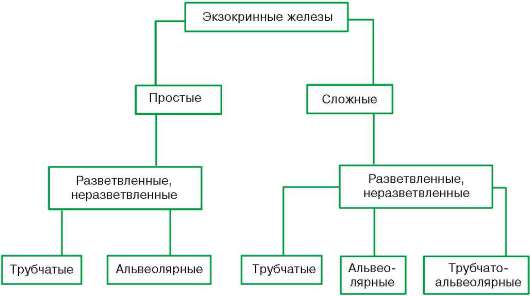
Scheme 6.2. Morphological classification of exocrine glands
types of epithelium depending on the origin of the glands. In glands formed from endodermal type epithelium (for example, in the pancreas), they are lined with single-layer cubic or columnar epithelium, and in glands developing from ectoderm (for example, in the sebaceous glands of the skin), they are lined with stratified epithelium. Exocrine glands are extremely diverse, differing from each other in structure, type of secretion, i.e., the method of secretion and its composition. The listed characteristics form the basis for the classification of glands. According to their structure, exocrine glands are divided into the following types (see Fig. 6.10, a, b; diagram 6.2).
Simple tubular glands have a non-branching excretory duct, complex glands have a branching one. In unbranched glands one at a time, and in branched glands several terminal sections open into it, the shape of which can be in the form of a tube or a sac (alveolus) or an intermediate type between them.
In some glands derived from ectodermal (stratified) epithelium, for example in salivary glands, in addition to secretory cells, there are epithelial cells that have the ability to contract - myoepithelial cells. These cells, which have a process form, cover the terminal sections. Their cytoplasm contains microfilaments containing contractile proteins. Myoepithelial cells, when contracting, compress the end sections and, therefore, facilitate the release of secretions from them.
The chemical composition of the secretion may be different; therefore, the exocrine glands are divided into protein(serous), mucous membranes(mucosal), protein-mucosal(see Fig. 6.11), greasy, salty(sweat, tears, etc.).
Two types of secretory cells may be present in the mixed salivary glands - protein(serocytes) and mucous membranes(mucocytes). They form
There are protein, mucous and mixed (protein-mucous) terminal sections. Most often, the composition of the secretory product includes protein and mucous components with only one of them predominant.
Regeneration. In the glands, in connection with their secretory activity, processes constantly occur physiological regeneration. In merocrine and apocrine glands, which contain long-lived cells, restoration of the original state of secretory epithelial cells after secretion from them occurs through intracellular regeneration, and sometimes through reproduction. In holocrine glands, restoration is carried out due to the proliferation of cambial cells. The newly formed cells are then transformed into glandular cells through differentiation (cellular regeneration).
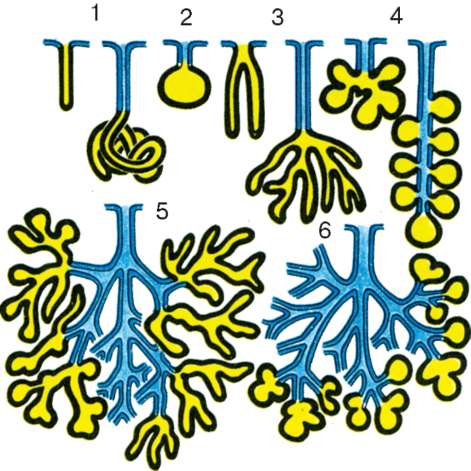
Rice. 6.11. Types of exocrine glands:
1 - simple tubular glands with unbranched end sections;
2 - simple alveolar gland with an unbranched end section;
3 - simple tubular glands with branched end sections;
4 - simple alveolar glands with branched terminal sections; 5 - complex alveolar-tubular gland with branched end sections; 6 - complex alveolar gland with branched end sections
In old age, changes in the glands can be manifested by a decrease in the secretory activity of glandular cells and changes in the composition
secretions produced, as well as weakening of regeneration processes and proliferation connective tissue(gland stroma).
Security questions
1. Sources of development, classification, topography in the body, basic morphological properties of epithelial tissues.
2. Multilayer epithelia and their derivatives: topography in the body, structure, cellular differential composition, functions, patterns of regeneration.
3. Single-layer epithelia and their derivatives, topography in the body, cellular differential composition, structure, functions, regeneration.
9. Glandular epithelium. Classification of glands. Phases of secretion. Types of secretion
Glandular epithelium is characterized by a pronounced secretory function. The glandular epithelium consists of glandular, or secretory, cells - glandulocytes. They carry out the synthesis and isolation of specific products - secrets to the surface: skin, mucous membranes and in the cavity of a number of internal organs [this is external (exocrine) secretion] or into the blood and lymph [this is internal (endocrine) secretion]. Through secretion, many important functions are performed in the body: the formation of milk, saliva, gastric and intestinal juice, and bile.
Most glandulocytes are distinguished by the presence secretory inclusions in the cytoplasm, developed endoplasmic reticulum and Golgi apparatus, as well as a polar arrangement of organelles and secretory granules.
Glandulocytes lie on the basement membrane. Their shape is very diverse and varies depending on the phase of secretion. In the cytoplasm of glandulocytes, which produce protein secretions (for example, digestive enzymes), a granular endoplasmic reticulum is well developed. In cells that synthesize non-protein secretions (lipids, steroids), an agranular endoplasmic reticulum is expressed. Numerous mitochondria accumulate in places of greatest cell activity, i.e. where the secretion is formed. The number of secretory granules in the cytoplasm of cells fluctuates in connection with the phases of the secretory process.
The cytolemma has a different structure on the lateral, basal and apical surfaces of cells. On the lateral surfaces it forms desmosomes and tight locking junctions. The latter surround the apical (apical) parts of the cells, thus separating the intercellular gaps from the lumen of the gland. On the basal surfaces of cells, the cytolemma forms a small number of narrow folds that penetrate the cytoplasm. Such folds are especially well developed in the cells of the glands that secrete a secretion rich in salts, for example, in the duct cells of the salivary glands. The apical surface of the cells is covered with microvilli.
Periodic changes in the glandular cell associated with the formation, accumulation, release of secretion and its restoration for further secretion are called secretory cycle: intake of substances - synthesis and accumulation of secretions - excretion of secretions.
To form secretions from the blood and lymph, various inorganic compounds, water and low molecular weight organic substances: amino acids, monosaccharides, fatty acids enter the glandular cells from the basal surface. Sometimes larger molecules of organic substances, such as proteins, penetrate into the cell by pinocytosis. Secrets are synthesized from these products in the endoplasmic reticulum. They move through the endoplasmic reticulum to the Golgi apparatus, where they gradually accumulate, undergo chemical rearrangement and form into granules that are secreted from glandulocytes. An important role in the movement of secretory products in glandulocytes and their secretion belongs to the cytoskeletal elements - microtubules and microfilaments.
However, the division of the secretory cycle into phases is essentially arbitrary, since they overlap each other. Thus, the synthesis of secretion and its release proceed almost continuously, but the intensity of secretion may either increase or decrease. In this case, the release of secretion (extrusion) can be different: in the form of granules or by diffusion without forming into granules, or by converting the entire cytoplasm into a mass of secretion. For example, after eating in the pancreas, all secretory granules are quickly released from the glandular cells, and then, within 2 hours or more, the secretion is synthesized in the cells without forming into granules and is released diffusely.
The mechanism of secretion in different glands is not the same, and therefore they distinguish three types of secretion:
merocrine (or eccrine),
apocrine and
holocrine.
At merocrine type of secretion, glandular cells completely retain their structure (for example, cells of the salivary glands). At apocrine type of secretion, partial destruction of glandular cells (for example, mammary gland cells) occurs, i.e. together with the secretory products, either the apical part of the cytoplasm of the glandular cells or the tips of the microvilli are separated. Third, holocrine the type of secretion is accompanied by the accumulation of secretion in the cytoplasm and the complete destruction of glandular cells (for example, cells of the sebaceous glands of the skin).
Restoration of the structure of glandular cells occurs either through intracellular regeneration (with mero- and apocrine secretion), or through cellular regeneration, i.e. division and differentiation of cambial cells (during holocrine secretion).
Glands
Glandular epithelial tissue forms glands - organs consisting of secretory cells that produce and secrete specific substances of various chemical natures. The secretions produced by the glands are important for the processes of digestion, growth, development, interaction with the external environment and others. Many glands are independent, anatomically formed organs (for example, the pancreas, large salivary glands, the thyroid gland), some are only part of the organs (for example, the stomach glands).
CLASSIFICATION OF GLANDS
There are three groups of glands.
1. Exocrine ( exocrine glands) having excretory ducts into the cavity: - large glands of the oral cavity; - small glands of the oral cavity and gastrointestinal tract; - liver.
2. Endocrine(endocrine glands), which do not have excretory ducts and secrete their secretions directly into the blood and lymph: - pituitary gland; - pineal gland; - thyroid gland; - parathyroid glands; - adrenal glands.
3. Mixed, in which exocrine and endocrine parts are simultaneously present: - pancreas; - gonads.
Endocrine glands produce highly active substances - hormones, entering directly into the blood or lymph. Therefore, they consist only of glandular cells and do not have excretory ducts. All of them are part of the body's endocrine system, which, together with the nervous system, performs a regulatory function.
Exocrine glands produce secrets, released into the external environment, i.e. on the surface of the skin or in organ cavities lined with epithelium. Multicellular exocrine glands consist of two parts: secretory, or terminal, sections and excretory ducts. The terminal sections are formed by glandulocytes lying on the basement membrane. The excretory ducts are lined with different types of epithelia depending on the origin of the glands.
Based on the structure of the terminal sections, glands are distinguished: branched and unbranched, as well as tubular, alveolar or mixed.
Based on the structure of the excretory ducts, glands are distinguished: simple and complex. Simple glands have a non-branching excretory duct, complex glands have a branching one.
The glands open into the excretory duct - in unbranched glands one at a time, and in branched glands there are several terminal sections.
In some glands that are derivatives of ectodermal (stratified) epithelium, for example in salivary glands, in addition to secretory cells, there are epithelial cells that have the ability to contract - these are myoepithelial cells. These cells cover the terminal sections of the gland with their processes. Contractile proteins are present in their cytoplasm. Myoepithelial cells, when contracting, compress the end sections and, therefore, facilitate the release of secretions from them.
The chemical composition of the secretion can be different; therefore, exocrine glands are divided into several types:
saline (for example: sweat and tears).
proteinaceous (or serous),
mucous membranes,
protein-mucous (or mixed),
10. Mesenchyme: sources of formation, structure, differentiation and functions.
Mesenchyme is an embryonic rudiment that serves as a source of development of connective tissue, blood, skeleton and smooth muscle tissue. Mesenchyme consists of loosely lying cells with processes and intercellular fluid located in the primary body cavity in the spaces between the germ layers. Mesenchyme (from the Greek mesos - middle and enchyma - contents, filling mass) is one of the embryonic primordia, representing the loosened part of the middle germ layer, or mesoderm. In vertebrates, mesenchyme arises from somites in places of loosening of their areas - dermatomes and sclerotomes, as well as as a result of the eviction of cells from the visceral and parietal layers of splanchnotomes. Coming from the dermatomes, the mesenchyme differentiates into the connective tissue base of the skin (the skin itself, or dermis). Sclerotomes give rise to skeletogenic mesenchyme, which differentiates into cartilage and bone tissue. Mesenchyme cells moving out of splanchnotomes form connective tissue, blood and lymphatic vessels, blood and lymph cells, and smooth muscle tissue of the viscera. Thus, in vertebrates, M. as a whole is the rudiment of the entire vast group of tissues of the internal environment. Developing from it is smooth muscle tissue in many properties it is closer to connective tissue than to musculoskeletal tissue. In vertebrates and humans, some part of the muscle is formed not from the mesoderm, but from the neuroectodermal rudiment, namely the neural crest, or ganglion plate (ectomesenchyme, or neuromesenchyme). From it arise chromatophores (pigment cells), some laryngeal cartilage, possibly dental pulp and dentin-forming cells (odontoblasts). Mesenchyme during its emergence consists of process cells connected in a reticulum by processes. The spaces between cells are filled with intercellular fluid. Individual cells can, by absorbing processes, be released from connection with other cells and, moving amoeboidally with the help of pseudopods, phagocytose bacteria and other foreign particles that have entered the body of the embryo. Thus, M. consists of fixed (sedentary) and mobile cells that can transform into each other. Together with the intercellular fluid, they make up the internal environment of the embryo. At the first stages of development, mesenchyme is still devoid of special tissue structures (fibers, etc.) and represents an embryonic rudiment, not tissue. However, its individual sections (especially those that are part of the provisional auxiliary organs of the embryo) very early undergo tissue specialization, turning into embryonic connective tissue, blood cells, etc. According to most histologists, vascular endothelium also develops from M. However, some They consider it to originate from a special vascular rudiment - the angioblast, the cells of which, mixed with M., are externally indistinguishable from its cells. Already in the embryo, all the mesenchyme is spent on the formation of tissues. Cambial (poorly differentiated) cells of the connective tissue of a child and an adult organism are qualitatively different from the m. of the embryo in a relatively higher level of differentiation. Therefore, the idea of “adult mesenchyme” or “mesenchymal reserve” is untenable: unchanged cells of the embryo are not preserved in a differentiated organism
Mesenchyme
Sources of mesenchyme formation
Dermatome
Sclerotome
Visceral layer of splanchnotome
Neural crest (Ganglion plate)
Various areas of mesoderm
Neuromesenchyme (ectomesenchyme)
Heterogeneity of mesenchyme
Due to the difference in the sources of its origin and unequal in its differentiation potential
Differentiations
Endothelium
All types of internal tissues
Smooth muscle tissue of the splanchnic (visceral) type
Glial macrophages (microglial cells) of nervous tissue
Tissues of the internal environment (Connective tissues)
General properties
mechanical
trophic
protective
homeostatic
transport (blood)
Main types of connective tissues
Normally they have no contact with the external environment
Lack of polarity (cells)
Developed intercellular substance
There are motile cells
The common source of development in ontogenesis is mesenchyme
Basic General Functions:
