Examples of types of connections of skeletal bones. Continuous connections of bones - synarthrosis
There are two main types of bone connections: continuous and discontinuous.
Continuous connections characterized by limited range of movements and relatively low mobility. Depending on the nature of the tissue that connects the bones, continuous connections are divided into three types: syndesmoses (junctura tibrosa) - connection of bones with connective tissue, synchondrosis (junctura cartilaginea) - connection of bones with cartilage tissue and synostosis - connection of bones with bone tissue.
Syndesmoses include all ligaments connecting bones to each other (ligaments between processes, vertebral bodies, etc.), membranes (interosseous membranes between the diaphyses of the bones of the forearm and lower leg, the membrane between occipital bone and I cervical vertebra), seams (layers connective tissue between the bones of the skull), as well as ligaments that strengthen the capsules of discontinuous joints - joints.
Connective tissue in continuous joints is most often dense and formed. In some cases, it consists of elastic fibers (yellow ligaments between the vertebral arches).
Synchondroses are elastic joints. The cartilage tissue connecting the bones can be of two types: hyaline cartilage (for example, the connection between the first rib and the sternum) and fibrous cartilage (the connections between the bodies of adjacent vertebrae - intervertebral cartilage).
Synostosis is the result of fusion of bones or their parts that were previously separate from each other (for example, fusion of the diaphysis with the epiphyses in an adult and the formation of a long bone).
The three types of continuous connections correspond to three stages in skeletal development. Syndesmoses correspond to the membranous stage, synchondrosis to the cartilaginous stage, and synostosis to the bone stage. Like the stages in the development of the skeleton, these types of joints can replace each other during a person’s life: syndesmoses turn into synostoses (fusion of the bones of the skull roof in the elderly and old age- the connective tissue of the sutures is replaced by bone tissue), synchondrosis turns into synostosis (cartilaginous tissue between the bodies of the sphenoid and occipital bones is replaced by bone - a single main bone is formed).
Half-joints- This is a transitional form of connections between continuous and discontinuous. In the semi-joints between the bones there is cartilaginous tissue, in the thickness of which there is a cavity, but there is no articular capsule and articular surfaces covered with cartilage (the pubic symphysis, the connection of the sacrum with the body of the first coccygeal vertebra).
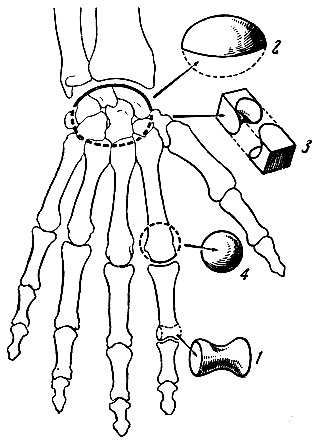
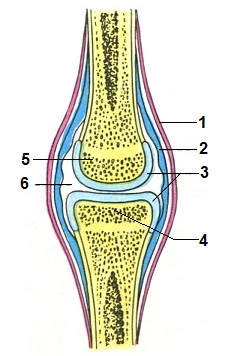
Intermittent connections, or joints, are the most complex form of movable bone joints. Each joint (articulatio) has three main elements (Fig. 55): articular surfaces, articular capsule and articular cavity.
The articular surfaces of bones that articulate with each other are covered with articular cartilage *.
* (Articular cartilages are usually hyaline; In some joints, such as the temporomandibular and acromioclavicular joints, the articular surfaces are covered with fibrocartilage.)
The joint capsule (capsule) consists of outer (fibrous) and inner (synovial) layers. The fibrous layer is made of dense connective tissue, and the synovial layer is made of loose connective tissue. Synovial fluid (synovium) is secreted from the synovial layer of the joint cavity, which provides lubrication of the contacting articular surfaces.
The articular cavity is limited by the articular capsule and the articular surfaces of the articulating bones. This slit-like space contains a small amount of synovial fluid.
In addition to the three main elements that form the joint, there is also an auxiliary apparatus: articular ligaments, articular discs and menisci, and synovial bursae.
Articular ligaments are made of dense connective tissue. In most cases, they are formed by thickenings of the fibrous layer of the joint capsule. Less common are independent ligaments running near the joint. Some joints have ligaments located in the articular cavity.
Accordingly, a distinction is made between extra-articular and intra-articular ligaments.
Articular discs and menisci are made of cartilage and are located in the articular cavity between the articular surfaces of the articulating bones. The discs are represented by solid plates, and the menisci have a crescent shape. Both play a large role in the movements of joints, the articular surfaces of which do not quite correspond to each other in shape.
Synovial bursae (bursae synoviales) are bag-like inversions of the synovial layer of the joint capsule: the synovial membrane, protruding through a thinned area of the fibrous layer of the joint capsule, forms a bursa located under the tendon or muscle, which are located directly at the joint. Synovial bursae reduce friction between tendons, muscles and adjacent bone.
It is necessary to distinguish mucous bursae (bursae mucosae) from synovial bursae, which, unlike the former, do not communicate with the articular cavity. The mucous bursae contain a small amount of fluid similar to the synovial fluid of joints.
Joint shapes
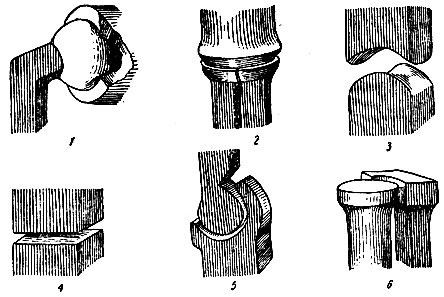
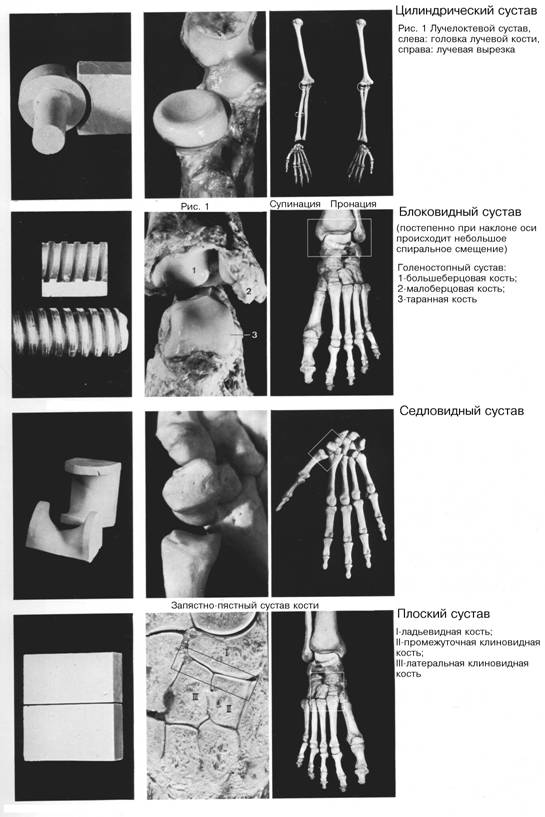
In accordance with the shape of the articulating surfaces, joints are distinguished: cylindrical, block-shaped, ellipsoidal, saddle-shaped and spherical (Fig. 56, 57).
The shape of the articular surfaces largely determines the nature of movement and the degree of mobility of the joints. Movements in the joints can be carried out around one, two or three axes. In accordance with this, uniaxial, biaxial and triaxial (multiaxial) joints are distinguished.
To uniaxial joints belong to cylindrical and trochlear joints; A type of trochlear joint is the helical joint.
A cylindrical joint is characterized by cylindrical articular surfaces (Fig. 56), which are located on the lateral surfaces of the bones, and their axis of rotation coincides with the length of the bones. Thus, in the joints between the radius and ulna bones, movement occurs around an axis running along the forearm. The radius rotates around the stationary ulna; turning outward is called supination, and turning inward is called pronation.
The trochlear joint, like the previous one, has cylindrical articular surfaces. However, the axis of rotation in it runs perpendicular to the length of the articulating bones and is located in frontal plane. Flexion and extension occur around this axis.
On one of the articular surfaces (concave) there is a comb, and on the other (convex) there is a guide groove corresponding to this comb, in which the comb slides. Thanks to the presence of ridges and grooves, a block is obtained. An example of such a joint is the interphalangeal joint of the fingers.
The helical joint has the structural features of a trochlear joint. However, the guide groove is not located perpendicular to the axis of the joint (as in the trochlear joint), but at a certain angle to it (humeral-ulnar joint).
To biaxial joints belong to the ellipsoidal and saddle joints.
An ellipsoidal joint has articular surfaces, one of which is convex and resembles in its shape part of an ellipsoid (Fig. 57), and the other is concave and corresponds in curvature to the first (for example, the wrist joint). Movements occur around two mutually perpendicular axes. Around frontal axis flexion and extension occur, and around the sagittal there is adduction and abduction *.
* (The movement during which a limb or part of a limb approaches the body is called adduction. Movement in the opposite direction is called abduction.)
Saddle joint (eg carpometacarpal joint thumb brushes), like the previous one, has two axes of rotation. Each articular surface is convex along one axis and concave along the other, so that the resulting surface resembles the surface of a saddle.
In biaxial joints, peripheral movement is also possible - movement around transitional axes.
Triaxial joints include ball-and-socket joints and their varieties (nut-shaped and flat).
The ball-and-socket joint has a spherical head and a socket corresponding to it in shape, and the dimensions of the articular surface of the socket are significantly smaller than the dimensions of the articular surface of the head, which provides a large range of movements in the joint (shoulder joint). In the nut joint ( hip joint) the articular fossa is deep, covering the head for more than half of its circumference, and therefore movements in the joint are limited. In a flat joint (for example, the articulation between the articular processes of the vertebrae), the curvature of the articular surfaces, which are small areas of the surface of a ball with a very large radius, is negligible. In such joints, the articular capsule is attached along the edge of the articular surfaces, so movements here are sharply limited and are reduced to a slight sliding of one articular surface around the other. Flat joints are inactive.
Movements in the ball and socket joint are carried out around the following axes: frontal (flexion and extension), sagittal (adduction and abduction) and vertical (rotation). In addition, peripheral movement is possible in the ball and socket joint. The essence of peripheral movement is that the limb making this movement describes a figure resembling a cone.
It should be noted that, in addition to the three axes mentioned, many other axes can be drawn through the center of the ball-and-socket joint, so such a joint is actually multi-axial, which provides it with greater freedom of movement.
Under normal conditions, the articular surfaces of the articulating bones are tightly adjacent to each other. They are held in this position (at rest and in motion) by three factors: 1) negative pressure in the joint cavity relative to atmospheric pressure; 2) constant muscle tone; 3) ligamentous apparatus of the joint.
In a hermetically sealed joint cavity the pressure is below atmospheric. As a result, the mating surfaces are pressed against each other.
Muscles take part in strengthening the joints, thanks to the constant traction of which the articular surfaces are adjacent to each other. Thus, in the shoulder joint, the muscles play the main role in holding the articular surfaces close to each other, so the “looseness” of the joint becomes understandable when the corresponding muscles are paralyzed, which under normal conditions provide movement in this joint.
The ligaments of the joints play an important role. Ligaments not only hold the articulating bones in their position, but also act as brakes that limit the range of movement. Thanks to ligaments, movements in the joints occur in certain directions. Thus, in a trochlear joint (for example, in the interphalangeal joint), ligaments are located on the sides of the joint and limit the displacement of the phalanges of the fingers to the sides. When, under the influence of mechanical reasons (fall, blow, etc.), movements occur in the joint that go beyond the limits of what is possible, the ligaments are damaged (sprain, rupture); in this case, the articulating ends of the bones can shift and joint dislocations occur.
Simple, complex and combined joints
Simple joints are formed by two bones. An example is the trochlear joint between the phalanges of the fingers (interphalangeal) or the ball-and-socket joint (shoulder). Despite their different anatomical and functional properties, both joints are simple, since only two bones are involved in their formation. Compound joints are formed by more than two bones. Thus, the humerus, ulna and radius bones articulate at the elbow joint.
A combined joint is a functional concept. A combined joint is understood as anatomically separate but functionally connected joints. For example, movements lower jaw occur simultaneously in both temporomandibular joints, which constitute one combined joint.
There are two main types of bone joints: continuous And intermittent, or joints. Continuous connections are present in all lower vertebrates and in the embryonic stages of development in higher ones. When the latter form bone primordia, their original material (connective tissue, cartilage) is preserved between them. With the help of this material, bone fusion occurs, i.e. a continuous connection is formed. Discontinuous connections develop at later stages of ontogenesis in terrestrial vertebrates and are more advanced, as they provide more differentiated mobility of skeletal parts. They develop due to the appearance of a gap in the original material preserved between the bones. In the latter case, remnants of cartilage cover the articulating surfaces of the bones. There is a third, intermediate type of connection - semi-joint
Continuous connections. Continuous connection – synarthrosis, or fusion, occurs when the bones are connected to each other by connecting tissue. Movements are extremely limited or completely absent. Based on the nature of the connective tissue, connective tissue adhesions are distinguished, or syndesmoses(Fig. 1.5, A), cartilaginous adhesions, or synchondrosis, and fusion with the help of bone tissue - synostosis.
Syndesmoses There are three types: 1) interosseous membranes, for example between the bones of the forearm or
shins; 2) ligaments, connecting bones (but not connected to joints), for example, ligaments between the processes of the vertebrae or their arches; 3) seams between the bones of the skull.
Interosseous membranes and ligaments allow some displacement of the bones. At the sutures, the layer of connective tissue between the bones is very small and movement is impossible.
Synchondrosis is, for example, the connection of the first rib with the sternum through the costal cartilage, the elasticity of which allows some mobility of these bones.
Synostosis develop from syndesmoses and synchondroses with age, when the connective tissue or cartilage between the ends of some bones is replaced by bone tissue. An example is fusion of the sacral vertebrae and overgrown sutures of the skull. Naturally, there is no movement here.
3. Discontinuous (synovial) bone connections. The structure of the joint. Classification of joints according to the shape of the articular surfaces, the number of axes and function.
Intermittent connections. Intermittent connection – diarthrosis, articulation, or joint, characterized by a small space (gap) between the ends of the connecting bones. There are joints simple, formed by only two bones (for example, the shoulder joint), complex - when the joint includes a larger number of bones (for example, the elbow joint), and combined, allowing movement only simultaneous with movement in other anatomically separate joints (for example, the proximal and distal radioulnar joints). The composition of the joint includes: articular surfaces, the articular capsule, or capsule, and the articular cavity.
Articular surfaces connecting bones more or less correspond to each other (congruent). On one bone forming a joint, the articular surface is usually convex and is called heads. On the other bone a concavity corresponding to the head develops - depression, or hole Both the head and the fossa can be formed by two or more bones. The articular surfaces are covered with hyaline cartilage, which reduces friction and facilitates movement in the joint.
Bursa grows to the edges of the articular surfaces of the bones and forms a sealed articular cavity. The joint capsule consists of two layers. The superficial, fibrous layer is formed by fibrous connective tissue, merges with the periosteum of the articulating bones and has a protective function. The inner, or synovial, layer is rich blood vessels. It forms outgrowths (villi) that secrete a viscous liquid - synovia, which lubricates the articulating surfaces and facilitates their sliding. In normally functioning joints there is very little synovium, for example in the largest of them - the knee - no more than 3.5 cm 3. In some joints (the knee), the synovial membrane forms folds in which fat is deposited, which has a protective function here. In other joints, for example, in the shoulder, the synovial membrane forms external protrusions, over which there is almost no fibrous layer. These protrusions in the form bursae are located in the area of tendon attachment and reduce friction during movements.
Articular cavity called a hermetically closed slit-like space, limited by the articulating surfaces of the bones and the articular capsule. It is filled with synovium. In the articular cavity between the articular surfaces there is negative pressure (below atmospheric pressure). The atmospheric pressure experienced by the capsule helps strengthen the joint. Therefore, in some diseases, the sensitivity of the joints to fluctuations in atmospheric pressure increases, and such patients can “predict” weather changes. The tight pressing of the articular surfaces to each other in a number of joints is due to tone, or active muscle tension.
In addition to the obligatory ones, auxiliary formations may be found in the joint. These include articular ligaments and lips, intra-articular discs, menisci and sesamoids (from Arabic, sesamo– grain) bones.
Articular ligaments They are bundles of dense fibrous tissue. They are located in the thickness or on top of the articular capsule. These are local thickenings of its fibrous layer. By spreading over the joint and attaching to the bones, ligaments strengthen the joint. However, their main role is to limit the scope of movement: they do not allow it to go beyond certain limits. Most ligaments are not elastic, but are very strong. Some joints, such as the knee, have intra-articular ligaments.
Articular lips consist of fibrous cartilage, ring-shaped covering the edges of the articular cavities, the area of which they complement and increase. The labrum gives the joint greater strength, but reduces the range of motion (for example, the shoulder joint).
Discs And menisci They are cartilaginous pads - solid and with a hole. They are located inside the joint between the articular surfaces, and at the edges they grow together with the articular capsule. The surfaces of the discs and menisci repeat the shape of the articular surfaces of the bones adjacent to them on both sides. Discs and menisci promote a variety of movements in the joint. They are present in the knee and mandibular joints.
Sesamoid bones small and located near some joints. Some of these bones lie deep in the articular capsule and, increasing the area of the articular fossa, articulate with the articular head (for example, in the joint of the big toe); others are inserted into the tendons of the muscles that span the joint (for example, the patella, which is encased in the quadriceps tendon). Sesamoid bones are also auxiliary muscle formations.
Classification of joints is based on a comparison of the shape of articular surfaces with segments of various geometric figures of rotation resulting from the movement of a straight or curved line (the so-called generatrix) around a fixed conditional axis. Different forms of motion of the generating line give different bodies of rotation. For example, a straight generatrix, rotating parallel to the axis, will describe a cylindrical figure, and a generatrix in the form of a semicircle will produce a ball. The articular surface of a certain geometric shape allows movements only along the axes characteristic of this shape. As a result, joints are classified into uniaxial, biaxial and triaxial (or almost multiaxial).
Uniaxial joints may be cylindrical or block-shaped.
Cylindrical joint has articular surfaces in the form of cylinders, with the convex surface covered by a concave cavity. The axis of rotation is vertical, parallel to the long axis of the articulating bones. It provides movement along one vertical axis. In a cylindrical joint, rotation along the axis in and out is possible. Examples are the articulations between the radius and ulna bones and the joint between the epistrophic tooth and the atlas.
Trochlear joint is a type of cylindrical, differs from it in that the axis of rotation runs perpendicular to the axis of the rotating bone and is called transverse or frontal. Flexion and extension are possible at the joint. An example is the interflank joints.
Biaxial joints there may be saddle-shaped(in one direction the articular surface is concave, and in the other, perpendicular to it, it is convex) and ellipsoidal(articular surfaces are ellipsoidal). An ellipse as a body of rotation has only one axis. The possibility of movement in an ellipsoidal joint around the second axis is due to the incomplete coincidence of the articular surfaces. Biaxial joints allow movements around two axes located in the same plane, but mutually perpendicular: flexion and extension around the frontal axis, adduction (to the median plane) and abduction around the sagittal axis. An example of an ellipsoidal joint is the wrist, and a saddle joint is the carpometacarpal joint of 1 finger.
Triaxial joints They are spherical and flat.
Ball and socket joints – the most mobile joints. Movements in them occur around three main axes that are mutually perpendicular and intersecting in the center of the head: frontal (flexion and extension), vertical (inward and outward rotation) and sagittal (adduction and abduction). But an infinite number of axes can be drawn through the center of the articular head, which is why the joint turns out to be practically multi-axial. An example is the shoulder joint.
One of the varieties of the ball-and-socket joint is the nut-shaped joint, in which a significant part of the ball-and-socket joint is covered by the ball-and-socket joint and, as a result, the range of movement is limited. An example is the hip joint. Movements in it can occur in any plane, but the range of movements is limited.
Flat joint – This is a segment of a ball with a very large radius, due to which the curvature of the articulating surfaces is very insignificant: it is impossible to separate the head and the fossa. The joint is inactive and allows only slight sliding of the articulating surfaces in different directions. An example is the joint between the articular processes of the thoracic vertebrae.
In addition to the movements described, in biaxial and triaxial joints, a movement called circular motion is also possible. During this movement, the end of the bone opposite to that fixed in the joint describes a circle, and the bone as a whole describes the surface of a cone.
Half joint characterized by the fact that the bones in it are connected by a cartilaginous lining, which has a slit-like cavity inside. The joint capsule is absent. Thus, this type of connection represents a transitional form between synchondrosis and diarthrosis (between the pubic bones of the pelvis).
There are different types of bones in the body:
- motionless
- Semi-movable
- Movable
Fixed type bone connections are characteristic of bones (with the exception of the lower jaw) and. With this type of connection, it is as if, as a result, it is formed at the place of their connection. Fixed connection type – .
Rice. Fixed connection of the skull bones using sutures (sutures are marked in red).
At semi-movable type connections with each other. Semi-movably connected to each other as well.

Rice. The connection of the vertebrae in the spine by cartilaginous intervertebral discs (indicated in blue) is an example of a semi-movable joint.
Movable joints called bones. The joint is formed by two or, with each other, strong strands of connective tissue. If there are only two bones in a joint, then of them, a – . The head and cavity are covered on the outside ( articular) cartilage. It allows during operation of the joint. In addition, the joint surrounds. Its cells are secreted into the joint cavity ( articular), which is also necessary for the operation of the joint. In addition, it delivers to the cells, as in it.
Rice. Diagram of the structure of a joint.
The bones in the human body are not located isolated from each other, but are interconnected into one single whole. Moreover, the nature of their connection is determined by functional conditions: in some parts of the skeleton, movements between bones are more pronounced, in others - less. Also P.F. Lesgaft wrote that “in no other department of anatomy is it possible to so “harmoniously” and consistently identify the connection between form and function” (function). By the shape of the connecting bones, you can determine the nature of the movement, and by the nature of the movements, you can imagine the shape of the joints.
The main point when connecting bones is that they “are connected to each other in such a way that, with the smallest volume of the junction, there is the greatest variety and magnitude of movements with the greatest possible strength in the most advantageous counteraction to the influence of shocks and shocks” (P.F. Lesgaft) .
The whole variety of bone connections can be represented in the form of three main types: continuous connections - synarthrosis, discontinuous - diarthrosis and semi-continuous - hemiarthrosis (half-joints)
Continuous bone connections– these are connections in which there is no break between the bones; they are connected by a continuous layer of tissue (Fig. 5).
Rice. 5. Connective tissue connections
Intermittent connections- these are connections when there is a gap between the connecting bones - a cavity.
Semi-continuous connections- connections, which are characterized by the fact that in the tissue that is located between the connecting bones there is a small cavity - a gap (2-3 mm) filled with liquid. However, this cavity does not completely separate the bones, and the essential elements of a discontinuous connection are missing. An example of this type of joint is the joint between the pubic bones.
Depending on the nature of the tissue located between the connecting bones, there are continuous connections (Fig. 6):
a) with the help of connective tissue itself - syndesmoses,
b) cartilaginous – synchondrosis;
c) bone – synostosis.
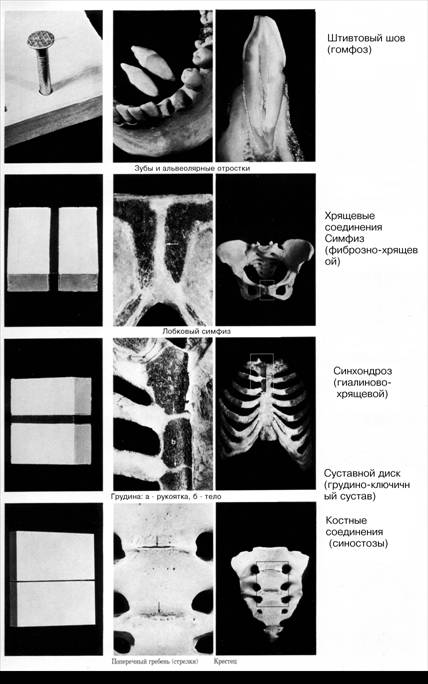
Rice. 6. Connective tissue connections – 2 (staple suture, cartilaginous connections)
Syndesmoses. If collagen fibers predominate in the connective tissue located between the bones, such connections are called fibrous, if elastic - elastic. Fibrous compounds, depending on the size of the layer, can be in the form of ligaments (between the processes of the vertebrae), in the form of membranes 3-4 cm wide (between the bones of the pelvis, forearm, lower leg) or in the form of sutures (between the bones of the skull), where the layer of connective tissue is only 2-3 mm. An example of continuous connections of the elastic type are the yellow ligaments of the spine, located between the vertebral arches.
Synchondroses. Depending on the structure of the cartilage, these connections are divided into connections using fibrous cartilage (between the vertebral bodies) and connections using hyaline cartilage (costal arch, between the diaphysis and the epiphysis, between individual parts of the skull bones, etc.).
Cartilaginous connections can be temporary (connections of the sacrum with the coccyx, parts of the pelvic bone, etc.), which then turn into synostoses, and permanent, existing throughout life (synchondrosis between temporal bone and occipital).
Hyaline compounds are more elastic, but fragile compared to fibrous ones.
Synostosis . These are connections of bones with bone tissue - ossification of epiphyseal cartilages, ossification of sutures between the bones of the skull.
Continuous bone connections (except synostoses) are mobile. The degree of mobility depends on the size of the tissue layer and its density. The connective tissue joints themselves are more mobile, the cartilaginous ones are less mobile. Continuous connections also have a pronounced property of shock absorption and shock absorption.
Discontinuous bone connections – these are connections that are also called synovial connections, cavitary connections or joints (Fig. 7, 8). The joint has its own specific design, location in the body and performs certain functions.

Rice. 7. Joints
Rice. 8. Joints
In each joint, basic elements and accessory formations are distinguished. The main elements of the joint include: the articular surfaces of the connecting bones, the articular capsule (capsule) and the articular cavity.
The articular surfaces of connecting bones must correspond to each other in shape to a certain extent. If the surface of one bone is convex, the surface of the other is somewhat concave. The articular surfaces are usually covered with hyaline cartilage, which reduces friction, facilitates the sliding of bones during movements, acts as a shock absorber and prevents fusion of bones. The thickness of the cartilage is 0.2-4 mm. In joints with limited mobility, the articular surfaces are covered with fibrocartilage (sacroiliac joint).
Bursa- This is a connective tissue membrane that hermetically surrounds the articular surfaces of the bones. It has two layers: the outer - fibrous (very dense, strong) and the inner - synovial (on the side of the joint cavity it is covered with a layer of endothelial cells that produce synovial fluid).
Articular cavity- a small gap between the connecting bones, filled with synovial fluid, which, by wetting the surfaces of the connecting bones, reduces friction, the force of adhesion of molecules to the surfaces of the bones strengthens the joints, and also softens shocks.
Additional formations are formed as a result of functional requirements, as a reaction to an increase and specificity of the load. Additional formations include intra-articular cartilage: discs, menisci, articular lips, ligaments, outgrowths of the synovial membrane in the form of folds, villi. They are shock absorbers, improve the congruence of the surfaces of connecting bones, increase mobility and variety of movements, and promote more uniform distribution pressure of one bone on another. Discs are solid cartilaginous formations located inside the joint (in the temporomandibular joint); The menisci have the shape of crescents (in knee joint); lips in the form of a cartilaginous rim surround the articular surface (near the glenoid cavity of the scapula); ligaments are bundles of connective tissue that go from one bone to another; they not only inhibit movements, but also direct them, and also strengthen the joint capsule; outgrowths of the synovial membrane are folds protruding into the joint cavity, villi filled with fat.
The joint capsule, ligaments, muscles surrounding the joint, atmospheric pressure (negative pressure inside the joint) and the adhesion force of synovial fluid molecules are all factors that strengthen joints.
Joints perform mainly three functions: they help maintain the position of the body and its individual parts, they participate in the movement of parts of the body in relation to each other, and, finally, they participate in locomotion - the movement of the entire body in space. These functions are determined by the action of active forces - muscles. Depending on the nature of muscle activity in the process of evolution, compounds were formed various shapes, having various functions.
), diarthrosis (synovial joints, juncturae synovialis), or joints (articulatio)
CONTINUOUS CONNECTIONS (SYNARTHROSES), SYNARTHROSIS
Depending on the nature of the tissue that connects the bones, four groups of continuous bone connections are distinguished - fibrous, cartilaginous, bone and muscle(Fig. 4.4).
I. Fibrous compounds - syndesmoses, juncturae fibrosae, or connections using connective (fibrous) tissue. These include ligaments, membranes, fontanels, sutures and impactions.
Ligaments,ligamenta- these are connections with the help of connective tissue, which look like bundles of collagen or elastic fibers and serve to strengthen the joints of bones. They can be very short, connecting adjacent bones, for example, interspinous, intertransverse ligaments, most ligaments of limb bones, and long, connecting several bones over a long distance (posterior and anterior longitudinal ligaments of the spinal column, supraspinous ligament). A special type of ligament is the yellow ligament, ligamenta flava formed by elastic fibers.
Membranes,membranae- these are connecting plates stretched between the diaphyses of long tubular bones. Their role is in many ways similar to ligaments. They also hold bones in relation to each other (intercostal membranes, interosseous membranes of the forearm and lower leg), serve as the origin of muscles, and form openings for the passage of blood vessels and nerves (obturator membrane).
fontanelles,fonticuli- these are connective formations that create conditions for displacement of the skull bones during childbirth and contribute to intensive bone growth after birth. In areas where several bones converge, there are 6 fontanelles covered by connective tissue plates: 2 unpaired (anterior or frontal, and posterior or occipital) and 2 paired (sphenoid and mastoid). The fontanelles are eliminated due to the proliferation of the skull bones and the formation of suture connective tissue between them.
Rice. 4.4. Continuous bone connections and semi-joints.
A - syndesmosis, interosseous membrane of the forearm (1); B - synchondrosis, intervertebral disc (2); B - semi-joint, pubic symphysis (3).
seams,suturae- These are thin layers of connective tissue located between the bones of the skull. Depending on the shape of the skull bones, the following sutures are distinguished: serrated - sutura serrata(between the bones of the cranial vault, for example, frontal and parietal), squamosal - sutura squamosa(between the edges of the temporal and parietal bones) and flat - sutura plana(between the bones facial skull, for example, nasals). The sutures serve as a growth zone for the bones of the skull and have a shock-absorbing effect during movements, protecting the brain, organs of vision, organs of hearing and balance from damage.
Injection,gomphosis- this is a special type of fibrous connection of teeth with the cells of the alveolar processes of the jaws with the help of dense connective tissue - periodontium, which has special purpose. This is a very strong connection that has a pronounced shock-absorbing property when loaded on the teeth.
II. Cartilage joints - synchondroses, juncturae cartilagineae, are connections between bones using cartilage tissue. The main purpose of synchondrosis is to soften shocks and stresses under heavy loads on the bone (shock absorption) and ensure a strong connection between the bones. At the same time, they have great mobility (for example, various movements in the spinal column).
According to the duration of existence of synchondrosis, they can be permanent(remain throughout a person’s life) and temporary(existing until a certain age, and then replaced by bone tissue). Permanent cartilages (connections with fibrocartilage) are the cartilages that form the intervertebral discs, the cartilages located between the pyramid temporal bone and neighboring bones - the sphenoid, occipital, as well as the anterior cartilaginous ends of the ribs. Temporary (connections with hyaline cartilage) synchondroses are metaepiphyseal cartilages, cartilages between individual parts of bones (pelvic), cartilage between the main part of the occipital and the body of the sphenoid bones.
If the temporary continuous connection is replaced by bone tissue, it is called synostosis.
III. Bone joints - synostoses, synostosis- connections using bone tissue that occur at the site of a temporary connection. These are the strongest connections from the group of continuous ones. They have completely lost their elasticity and shock-absorbing properties (for example, connections between individual bones of the base of the skull, halves of the lower jaw, between the sacral vertebrae, bones that make up the pelvic bone, etc.)
IV. Muscle joints - synmioses (synsarcoses), synmyosis, - connections between bones using muscles. They strengthen the joint, hold the articular surfaces of the bones relative to each other, thanks to constant muscle tone. An example is muscles shoulder girdle (mm. cinguli membri superioris). They form a discontinuous muscle junction ( synsarcosis) , attaching the spatula and humerus To chest and cervical vertebrae.
Half-joints (hemiarthrosis), haemiarthrosis
Half-joints or symphyses, symphysis(from Greek: symphysis- fusion) - are cartilaginous connections, which are an intermediate type of connection between continuous and discontinuous connections. The symphyses contain cartilage located between two bones, in which there is a small slit-like cavity. The walls of this cavity do not have a synovial lining, and the cavity itself is not filled with synovial fluid.
An example of this connection is the symphysis of the manubrium of the sternum, symphysis manubriosternalis, intervertebral symphysis, symphysis intervertebralis, and pubic symphysis, symphysis pubica. In some cases, symphyses are formed at the connection of the V lumbar and I sacral vertebrae, as well as between the sacrum and coccyx.
INTERRUPTIVE CONNECTIONS (DIARTHROSES), DIARTHROSIS
Discontinuous joints are joints or synovial joints. joint,articulatio- This is a type of connection of bones, characterized by great mobility and a variety of movements.
Each joint is a discontinuous connection of bones that includes four main elements of joints(Fig. 4.5):
1. Articular surfaces covered with hyaline cartilage.
2. Articular capsule.
3. Joint cavity.
4. Joint fluid.

Rice. 4.5. Diagram of the structure of a joint.
1 - periosteum; 2 - bone; 3 - articular capsule; 4 - articular surfaces covered with articular cartilage; 5 - articular cavity.
1. Articular surfaces,facies articulare- These are areas of bone covered with articular cartilage. In most cases, when bones articulate, the articular surfaces correspond to each other, i.e. They congruent. If one articular surface is convex (articular head), then the second, articulating with it, is concave (glenoid cavity). In some joints these surfaces do not correspond to each other either in shape or size. Such joints are called incongruent.
articular cartilage, cartilago articularis, firmly connected to the bone. The role of articular cartilage is that it smoothes out the unevenness and roughness of the articular surfaces of the bones, giving them greater congruence. Due to its elasticity, it softens shocks and shocks. The greater the load a joint experiences from gravity, the greater the thickness of the articular cartilage on the articulating surfaces.
2. Articular capsule,capsula articularis- this is a bag that hermetically surrounds the articular cavity, growing at the edge of the articular surfaces or at a slight distance from them. It firmly fuses with the periosteum, forming a closed articular cavity. The capsule consists of an outer layer - a fibrous membrane, and an inner layer - a synovial membrane. fibrous membrane, membrane fibrosa, durable and thick.
In some places it thickens, forming ligaments that strengthen the capsule. The synovial membrane faces the joint cavity, is richly supplied with blood, and is lined from the inside with synoviocytes, which secrete synovial fluid, which has the properties of macrophages. The synovial membrane has numerous villi and folds that increase its surface.
3. Articular cavity,cavitas articularis- this is a hermetically sealed space, limited by the articular surfaces and capsule, filled with synovial fluid. The shape of the articular cavity depends on the shape of the articulating surfaces, the structure of the capsule, the presence or absence of auxiliary formations inside the joint (articular disc or meniscus) and intracapsular ligaments.
4. Joint fluid. Synovial fluid in its composition and nature of formation is a transudate - an effusion of blood plasma and lymph from the capillaries adjacent to the synovial membrane. Synovial fluid: lubricates articular surfaces (reduces friction during movements, increases gliding), adheres articular surfaces, softens the load, nourishes articular cartilage.
Auxiliary elements of joints. In addition to the main ones, joints also contain auxiliary elements of the joints, which ensure optimal joint function. The main ones are: extra-articular and intra-articular ligaments, intra-articular cartilage (articular disc and menisci), articular labrum, synovial folds, sesamoid bones, synovial bursae.
Ligaments serve as passive brakes, limiting movement in the joint. In relation to the joint cavity, they can be divided into intra- and extra-articular.
Extra-articular ligaments considered as capsule and extracapsular. Capsular ligaments are thickenings of the fibrous membrane. Ligaments can be located outside the capsule (without merging with it), and then they are called extracapsular.
Intra-articular ligaments,ligamenta intraarticularia, are fibrous ligaments covered with a synovial membrane that connect the articular surfaces in the knee joint (cruciate ligaments of the knee joint), in the joint of the rib head and in the hip joint.
Intra-articular cartilage, сartilago intraarticulares, are fibrous cartilages located between the articular surfaces in the form of cartilaginous plates - discs and menisci:
- articular disc,discus articularis, is a cartilaginous plate that divides the joint into two floors. In this case, two separated cavities are formed, as, for example, in the temporomandibular, sternoclavicular and acromioclavicular joints;
- articular meniscus, meniscus articularis, - the plates have a semi-lunar shape (lat. menisci- crescent) and the edges are fused with the capsule (for example, the knee joint), the joint cavity is only partially divided by cartilage plates. Discs and menisci ensure congruence of the articular surfaces, soften shocks, and reduce pressure on the underlying articular surfaces.
Articular lip,labrum articulare,- This is a cartilaginous rim that complements the articular fossa along the edge. The labrum is found in two joints: the shoulder and the hip ( labrum glenoidale et labrum acetabulare). It increases the area of the articular surface, makes it deeper, thereby limiting the range of movements.
Synovial folds, plicae synoviales,- These are connective tissue formations rich in blood vessels that fill the free spaces of the joint cavity. If fatty tissue accumulates inside them, fat folds form. Folds help reduce the joint cavity and increase range of motion.
Sesamoid bones, ossa sesamoidea,- These are intercalary bones that are closely connected to the joint capsule and the muscle tendons surrounding the joint. They help reduce the joint cavity and indirectly increase the range of motion in this joint. The largest sesamoid bone is the patella. Small sesamoid bones are often found in the joints of the hand and foot, for example, in the interphalangeal joint, carpometacarpal joint of the first finger, etc.
Synovial bursae, bursae synoviales, are small cavities that communicate or do not communicate with the joint cavity. The largest number of them is found in the knee joint. Synovial fluid accumulates inside them, which lubricates nearby tendons.
