Dangerous and especially dangerous human diseases. Viral outbreaks: which diseases are common where? Reminder for tourists
Illustration copyright Getty
Epidemics of terrible diseases threaten not only humans. Our little brothers are sometimes literally mowed down by approximately the same serious illnesses- from Ebola fever and anthrax to cancer and plague, says the correspondent.
Outbreaks of deadly diseases can wipe out thousands of animals in a very short time. The situation becomes especially dangerous when it comes to rare or endangered species.
Over the past decades, many new animal diseases have emerged, and already known diseases have appeared in new territories. "This is partly due to increased trade and human migration, which allows pathogens to spread across different regions," says Mayor Kilpatrick of the University of California, Santa Cruz. Infections are transmitted between people, domestic and wild animals.
The most serious threat to fauna continues to be habitat loss, often caused by the expansion of agricultural land. But diseases can also lead to a significant reduction or even extinction of wild animal populations, emphasizes Richard Cock of the Royal Veterinary College in Hatfield, England.
This article will discuss ten diseases that cause great harm to animals in the wild. Let's start our list with the infamous disease.
1. Ebola
Illustration copyright BSIP SA Alamy Image caption The Ebola virus is very dangerous for both chimpanzees and gorillas. It kills approximately 95% of infected individualsWe think of Ebola as a human disease, and there is an obvious explanation for this: the outbreak of this fever claimed about 10 thousand lives last year. But it also affected the populations of our closest relatives, the great apes.
In the early 1990s, Ebola wiped out flocks of chimpanzees in the Tai National Park in the African Ivory Coast. In the next decade, several outbreaks of the disease in the Republic of Congo seriously thinned the local gorilla population: in 2002-2003, the fever killed about 5,000 of those on the verge of extinction primates in the Lossi Nature Reserve, and then, in 2003-2004, destroyed hundreds of gorillas in the Odzala National Park.
The Ebola virus is very dangerous for both chimpanzees and gorillas. It kills approximately 95% of infected individuals, causing severe fever and bleeding.
This threat becomes even more serious when it is combined with other factors dangerous to great apes - poaching and deforestation. Uncontrolled hunting has reduced the numbers of gorillas and chimpanzees so much that Ebola could completely wipe out some populations, says Julia Jones of Bangor University in the UK.
One solution to the problem could be an Ebola vaccine. By 2014, scientists had tested the drug on a group of captive chimpanzees and it was found to be safe and effective.
2. Chytridiomycosis
Illustration copyright Chris Mattison Alamy Image caption A deadly fungus has caused a catastrophic decline in the populations of more than 200 amphibian species over the past 30 years.The deadly fungus chytridiomycetes has proven fatal to many frogs and salamanders. Over the past 30 years, it has caused a catastrophic decline in the population of more than 200 species of amphibians, and some of them eventually even became extinct.
For example, epidemics in Panama's El Cope National Park in the early 2000s wiped out 30 species. Five of them were previously unknown to science.
This fungus, with the Latin name Batrachochytrium dendrobatidis, is found on all continents except Antarctica. It affects the outer layer of amphibian skin. Because frogs and salamanders absorb nutrients and water through their skin, the infection kills them over time.
However, this fungus was not always so harmful. For more than 100 years, it did not cause any harm to amphibians in some of their habitats, for example, in the US state of Illinois and in Korea.
Not all infected species die from infection. Some of them, such as the American bullfrog and the African smooth clawed frog, are resistant to the dangerous fungus. These species are believed to have contributed to the spread of the disease, although, as Kilpatrick notes, international trade in amphibians also played a role.
3. West Nile encephalitis
Illustration copyright Dick Daniels CC by 3.0 Image caption Mosquito-borne virus has infected and killed millions of birds across the United States, Mexico and CanadaIn 1999, the American city of New York became the epicenter of an outbreak of a dangerous disease. People went to hospitals with encephalitis: their brains were inflamed. Around the same time, several city crows and other birds from the Bronx Zoo were found dead. In all these cases, the culprit was the West Nile encephalitis virus, which at that time was found mainly in Africa and Asia.
The mosquito-borne virus has since infected and killed millions of birds across the United States, Mexico and Canada. The virus has been found in 48 species of mosquitoes and 250 species of birds, and is sometimes transmitted to humans and horses.
In some areas, the disease has reduced the number of American ravens by 45%. The virus has also led to significant declines in the numbers of other bird species such as the wandering thrush, eastern sialia, sharp-crested tit and chickadee. However, according to Kilpatrick, they are not threatened with complete extinction from West Nile encephalitis.
However, other, rarer species are under threat. Scientists have developed an anti-encephalitis vaccine for the California condor and for the island scrub jay, which lives only on Santa Cruz Island off the southwest coast of the United States. Vaccines are now being tested for other bird species.
4. "White nose syndrome"
Illustration copyright Michael Durham NPL Image caption The White-nose Syndrome epidemic has killed nearly six million bats and reduced the number of some species by 99%In 2006, an amateur caver took a photograph of a bat in a cave near Albany in the US state of New York. The bat's nose was covered with white fungus. This image was the first photographic evidence of a dangerous epidemic affecting bats in North America. The disease, called “white nose syndrome,” quickly spread throughout the United States and Canada.
The epidemic has killed almost six million bats, and the number of some species - such as the North Queensland smooth-nosed bat - has declined by 99% in the north-east of the continent. "White-nose syndrome is having a serious impact on North American bat populations," Kok said.
Fungus, disease-causing, called Pseudogymnoascus destructans. It disrupts the hibernation of bats. Instead of sleeping in their caves, bats fly too far from the lair, even in daytime. They quickly deplete their reserves of subcutaneous fat and die of starvation.
The infection may have come from Europe, where it has no noticeable effect on local bats. dangerous influence. Restricting people's access to caves and protecting bat habitats are being considered as possible measures to combat the epidemic.
5. Anthrax (anthrax)
Illustration copyright Scott Camazine Alamy Image caption In 2004, in the Malilangwe Game Reserve in Zimbabwe, anthrax wiped out about 90% of the local population of wild herbivores.Anthrax is notorious as a weapon of bioterrorism. However, this disease has threatened the fauna from time immemorial. It mainly affects herbivores, but can also be transmitted to other mammals, including some carnivores, great apes and humans.
Anthrax infection can have different consequences, depending on the species of animal and the ecosystem in which the species lives. In areas such as Etosha National Park in Namibia, Africa, the disease is considered a naturally occurring environment, and attempts to combat it were abandoned in the early 1980s, says ecologist Wendy Turner of the University of Oslo in Norway.
However, from time to time, anthrax outbreaks become deadly. For example, in 2004, in the Malilangwe Nature Reserve in Zimbabwe, anthrax destroyed about 90% of the local population of wild herbivores. In 2010, a similar outbreak in Uganda killed more than 80 hippos.
Anthrax spores (Bacillus anthracis) can live in the soil for several years and infect grazing livestock, and through them, people. According to Turner, to combat the disease, it is worth regularly vaccinating domestic herbivores.
6. Facial tumor of the Tasmanian devil
Illustration copyright Dave Watts NPL Image caption Facial tumors were first noticed in Tasmanian devils in 1996, and have since wiped out up to 90% of some populations of these animals.A strange epidemic of a contagious cancer has broken out among Tasmanian devils living in Australia. This cancer is transmitted from one animal to another when they bite each other. And they often do this, fighting for food or sexual partners.
This disease is often fatal. Large cancerous tumors appear on the faces of infected devils, which subsequently spread throughout the body and kill the animal within a few months.
According to scientists, the disease initially appeared in the so-called Schwann cells nerve tissue only in one animal. However, later cancer cells began to spread from one Tasmanian devil to another, facilitated by the tendency of these animals to fight.
Genetically, all Tasmanian devils differ very little from each other, and, as a result, their immune systems are not able to provide strong resistance to cancer. The disease was first noticed in 1996, but has since wiped out up to 90% of some populations of these animals.
To protect the species, scientists have created “reserve populations” of approximately 500 healthy Tasmanian devils in captivity. Within these populations, 98% of the genetic diversity of the entire species is represented.
7. Canine distemper
Illustration copyright Steve Bloom Images Alamy Image caption In the late 2000s, canine distemper wiped out 49 of Tanzania's 52 captive wild dogs in just two months.The canine distemper virus, which originated in domestic dogs, is wiping out wild predators around the world. This virus is very similar to the causative agent of human measles; it affects the respiratory, nervous and digestive system animals.
In 1985, canine distemper struck black-footed ferrets in the US state of Wyoming. Then, in the early 1990s, it killed many wild dogs in Africa, as well as about 1,000 lions. And in the late 2000s, the virus killed 49 of 52 captive wild dogs in Tanzania in just two months.
As the number of domestic dogs grows, this disease spreads to new territories and is transmitted to an increasing number of species of predatory animals. It affected, in particular, the rare Amur tigers that live on Far East Russia.
Vaccinating domestic dogs can limit the spread of the virus to some extent. However, this is not quite enough, since other animals can also carry it. To save rare species, it may be necessary to undertake targeted vaccination.
8. Chlamydia
Illustration copyright Roland Seitre NPL Image caption Chlamydia has reduced the number of koalas in some areas of Australia from 60,000 in the mid-1990s to 10,000 in 2012.Australian koalas suffer from a sexually transmitted disease, chlamydia, which also affects humans. This disease can deprive an infected koala of the ability to reproduce and lead to genitourinary and respiratory systems, blind or even kill the animal.
Combined with drought, chlamydia has reduced koala numbers in some parts of Australia from 60,000 in the mid-1990s to 10,000 in 2012. The populations most affected were in the states of Queensland and New South Wales.
In order to detect infection early, some veterinarians resort to ultrasound scanning of animals instead of traditional smears. In addition, scientists have begun sequencing koala genes, including those that play a key role in their immune system. Experts hope to understand how the disease affects these genes.
The situation is complicated by another disease - a koala retrovirus, similar to the human immunodeficiency virus. It suppresses the immune system, making animals less resistant to chlamydia.
These two diseases, as well as the destruction of koala habitat and the threat from other species, have brought these cute animals to the brink of extinction. However, successful tests have already been carried out on a vaccine that may be able to save them.
9. Itchy scabies
Illustration copyright Juan Iacruz CC by 3.0 Image caption Mange is believed to have killed all the foxes on the Danish island of Bornholm.More than 100 species of animals are affected by this disease, from Australian wombats to European foxes and lynxes and North American wolves. A close relative of the animal scabies mite causes scabies in humans.
The mite bites under the skin, and the scabies it leaves become inflamed. The infection spreads through constant scratching. Over time, the animal may lose its fur, suffer from dehydration, hypothermia and hunger, and in some cases even die.
In many stable populations, mange does not have a long-term effect on animal numbers. But the disease could prove fatal to populations that are already endangered or isolated. For example, it is believed that all foxes on the Danish island of Bornholm died out from scabies.
10. Plague
Illustration copyright Charlie Summers N.P.L. Image caption In some areas of North America, the plague wiped out entire colonies of prairie dogs. The mortality rate from it is over 90%.The same bacterium that caused devastating plague epidemics in human civilization (including the European “Black Pestilence” of the mid-14th century) also wipes out representatives of the animal world. This is the plague bacillus Yersinia pestis.
Plague in animals was first observed in North America in the early 19th century. Perhaps ships coming from plague-stricken areas of Europe and Asia brought with them infected fleas and rats, which transmitted the plague bacillus to the local fauna, which had not previously encountered the plague.
In some areas of North America, the plague wiped out entire colonies of prairie dogs. The mortality rate from it in these animals was more than 90%.
The loss of prairie dogs has in turn led to a decline in the number of black-footed ferrets. One of the rarest species of North American animals, they feed primarily on prairie dogs and raise their young in their burrows. Therefore, ferrets depend on prairie dogs, not to mention the fact that the plague is also deadly for them.
The endangered ferrets have been bred in captivity and released back into the wild, and their numbers are slowly growing. Vaccinating ferrets and prairie dogs through vaccine baits can also help stop the spread of plague.
Illnesses of the expectant mother can have direct impact on the health and development of the fetus. Therefore, pregnant women pay increased attention to the condition of their body.
Most dangerous period- this is the first trimester. At this time, the fetus is at greatest risk. Therefore, many parents prefer to keep their pregnancy a secret for the first 3 months. After the first trimester, the child is no longer so vulnerable, but some diseases still threaten his development and even life.
Prevention and vaccination
Most often, pregnant women are worried about infections that they have never encountered before. Vaccination is one of the methods of prevention various diseases and may help prevent the onset of certain diseases.
Regular observation by a doctor, timely tests and following his recommendations are a guarantee of reducing the risk of spontaneous abortion and fetal infection during pregnancy.
18 most dangerous diseases for a pregnant woman
1. Urinary tract infections
The most common infections genitourinary tract during pregnancy are cystitis and thrush. They pose the greatest danger in the first and last trimester of pregnancy. In recent weeks, these diseases can lead to premature birth.
2. Gestational diabetes
This is the name for an increase in blood glucose levels in a pregnant woman. It is caused by insufficient production of insulin by the pancreas. Gestational diabetes does not threaten the baby. However, it can lead to the development of other types of diabetes in the expectant mother if appropriate measures are not taken.
3. Syphilis
One of the most easily transmitted diseases to the fetus. It can lead to miscarriage and stillbirth. The most commonly used therapy is penicillin.
4. Anemia
A common problem among pregnant women. Fortunately, it can be easily eliminated with a diet rich in iron. It is also possible to prescribe vitamins.
5. Measles
The consequences of measles in pregnancy can be premature birth, spontaneous abortion, or the development of chronic lung diseases. To avoid this, you need to get vaccinated against measles.
6. Genital herpes and chicken pox
These diseases are dangerous for both the child and the unborn fetus. Cataracts, insufficient development of tissues and organs, microcephaly and bone defects may occur. These consequences are most likely if a woman becomes ill in the first 20 weeks of pregnancy.
If infection occurs a month before birth, a cesarean section is prescribed to minimize the risk of infection of the child.
7. Rubella
Unfortunately, there is no therapy for this disease. Regular monitoring by a doctor is necessary in order to promptly identify possible developmental defects, including blindness, microcephaly, cardiovascular diseases and deafness.
8. Inflammation of the gums
Even ordinary gum inflammation can harm the fetus or lead to premature birth.
9. Vaginitis
Symptoms of this disease include discharge and a strong odor, but it is not a sexually transmitted disease. It's about about a disturbance in the vaginal flora, which can be triggered by ordinary stress or another factor that has weakened the body’s protective functions.
10. Cytomegalovirus
This infection affects the blood, so there is a high probability of transmitting the virus to a child. There is antiviral therapy, but it is better to prevent the expectant mother from becoming infected by avoiding eating poorly cooked meat and unwashed fruits and vegetables.
11. Toxoplasmosis
To avoid this disease, you should heat-treat meat and thoroughly wash vegetables and fruits. In addition, if you have animals in the house, especially cats, you should minimize contact with their feces. Ask other household members to change your pet's sand tray.
12. HIV
In some cases, a mother can choose a traditional birth without fear of infecting the baby. After birth, the baby is bathed to reduce the risk of infection through the blood, and drug therapy to prevent transmission of the virus. Breastfeeding is excluded, as the virus can be transmitted through breast milk.
13. Hepatitis B
About half of infected mothers pass the hepatitis B virus to their children. But regular monitoring by a doctor and following all his recommendations will help avoid this. Even before birth, immunoglobulin therapy is carried out, and after the child is born, he is vaccinated as quickly as possible to reduce the risk of transmission of the virus.
14. Hepatitis C
The main problem is that this virus quickly leads to liver cirrhosis and chronic hepatitis. For hepatitis C breast-feeding also not recommended.
15. Sexually transmitted diseases
The most common diseases in pregnant women are sexually transmitted diseases. There are antibiotics and antivirals which are prescribed in this case.
16. Pneumonia
One of the most dangerous diseases for both mother and child. This disease itself is difficult to treat, and pregnancy makes the condition worse. A pregnant woman, due to the general weakening of the body, is more likely to develop this complication in case of a common cold or flu.
17. Chikungunya
In our latitudes, this disease has never become widespread, unlike in warmer countries. However, do not forget about it if you plan to travel. Chikungunya is spread by mosquitoes, one bite of which can infect a pregnant woman. Although spontaneous miscarriages are quite rare in pregnant women with chikungunya, expectant mother, and the child after birth should regularly visit the doctor to minimize the risk of infection of the child.
It is still unknown how the virus works, but the risk of developing microcephaly is very high. It is transmitted in the same way as chikungunya, through mosquito bites, and recent years has reached epidemic proportions in some southern countries. So, if you are planning a visit to exotic places, it is better to clarify the epidemiological situation in this country.
Watch the video and learn more about infections during pregnancy.
1. Object, subject, methodology, theory and practice of life safety.
2. Life safety and risk theory.
3. Safety in various spheres of life.
4. Criteria for excessive and acceptable risk.
5. Dangerous and emergency situations (ES), their essence, dynamics and classification.
6. Emergencies natural nature and protection from their consequences.
7. Man-made emergencies and protection from their consequences.
8. Social emergencies and protection from their consequences.
9. National interests of Russia.
10. Modern terrorism. Methods to combat it.
11. Organization of security measures in institutions of various types.
12. Ensuring national security Russian Federation.
13. Civil defense and its main tasks.
14. Organization of evacuation measures in peacetime and wartime.
15. Protective structures for civil defense.
16. Personal protective equipment.
17. Negative factors habitats.
18. Subject, concept, main tasks of life safety in production.
19. Basic legislation of the Russian Federation on labor protection. Industrial safety.
20. Industrial sanitation, occupational hygiene and personal hygiene.
21. The concept of the first medical care. Providing first aid in terminal conditions.
22. Providing first aid for wounds and bleeding.
23. Providing first aid for thermal injuries.
24. Providing first aid for poisoning.
25. Basic principles of protecting the population during emergencies in peacetime and war.
26. Basic principles of preventing natural man-made emergencies.
27. Medical characteristics of wounds and first aid for wounds.
28. Electrical injury and first aid for electrical injuries.
29. First aid for prolonged tissue compression (crushing) syndrome.
30. Psychological aspects of survival in emergency situations.
31. First aid for emergency conditions and accidents. The concept of shock, signs of shock, simple anti-shock measures.
32. Modern means of destruction, the consequences of their use.
Approved at a department meeting
"Social science"
« 03 » September 2013
protocol no. 1
Head of the Department, Candidate of Psychology, Associate Professor
I.I. Patsakula
DANGEROUS AND ESPECIALLY DANGEROUS HUMAN DISEASES
Epidemic- This widespread infectious disease, significantly exceeding the level of incidence usually recorded in the given territory.
Pandemic occurs when human infectious diseases spread across a number of countries or an entire continent.
Epidemic process is the phenomenon of the emergence and spread of infectious diseases among people, representing a continuous chain of sequentially occurring homogeneous diseases. The conditions for the emergence and maintenance of the epidemic process are considered to be the presence of sources and routes of transmission of infection, human susceptibility to infection and a number of social factors.
Sources of infections can be infected people or
animals. The main routes of transmission of infection: airborne, food, water, vector-borne, i.e. through blood, and contact.
Human susceptibility to infection- this is the biological property of body tissues to be an optimal environment for the reproduction of a pathogen and to respond to its introduction by an infectious process.
Since infectious process flows into human society, social factors are of great importance: living conditions, level of sanitary
culture, medical care of the population, population density, material condition, public amenities, nature of nutrition, water supply, etc.
Infectious diseases occur more often if:
The level of sanitary culture is low;
Population density is high;
Sanitary and technological preparation rules are violated
and food storage (unwashed vegetables and fruits are consumed, water is taken from
random sources, etc.);
The rules of personal hygiene are not observed (washing hands before and after eating
going to the toilet, etc.).
Pathogens of dangerous and especially dangerous infections are characterized by:
High pathogenicity (the ability to cause diseases);
High resistance to environmental influences;
The ability to maintain viability and virulence for a long time (bo
beneficial properties) in water, food, on objects;
The ability to be transmitted from person to person in various ways;
ability to cause severe clinical forms of the disease, often accompanied
causing complications and leading to death
Some dangerous and especially dangerous human infectious diseases Plague - spicy infectious disease in humans and some animals, caused by the plague bacillus. This disease was called the "Black Death". If a plague appeared in the city, then a black flag was hung on the city wall, which symbolized that it was forbidden to approach the city. Humanity knows three plague pandemics (VI, XIV, XIX centuries). Developing shipping contributed to the passive migration of rats and the introduction of plague with them to various countries. For example, in 1347, an epidemic of bubonic plague began in Europe, which was brought from ships that came from overseas countries. When the epidemic ended three years later, it turned out that it had claimed a quarter of the European population - 25 million lives.
Clinically, the plague is characterized by general severe intoxication, severe damage to the cardiovascular system and local manifestations, which depend on the location of the pathogen.
Forms of plague: pneumonic (damage to the lungs), bubonic (defeat lymph nodes), bubonic skin (carbuncles and skin ulcers with damage to the lymph nodes).
Carbuncle- it's spicy purulent inflammation skin and subcutaneous tissue, coming from the hair follicles and sebaceous glands. Bubo is a painful enlarged lymph node.
All forms of plague quickly lead to death without special treatment. Probability of death - 90
The presence of natural foci of plague in Russia (Caspian, Transbaikal, etc.), the growth of international relations, military conflicts, and population migration currently force us to maintain constant anti-epidemic vigilance.
Treatment: antibacterial drugs, the choice and route of administration of which, as well as the volume of therapy in general, are determined by the form of the disease, the severity of its course, and the nature of complications.
Cholera- acute infectious intestinal disease human caused by Vibrio cholerae. Cholera is one of the oldest human diseases. To early XIX V. it was endemic (characteristic) for areas located in the river valley. Ganges and its tributaries. Subsequently, cholera periodically spread in many countries of the world, claiming millions of human lives. Cholera was brought to Europe in 1816. A total of seven devastating cholera pandemics have been described. The beginning of the 7th pandemic dates back to 1961. Total number only bacteriologically confirmed cases of disease, according to the World Organization. health care (WHO), by the beginning of 1984 exceeded 1.3 million people.
The clinically pronounced form of cholera is characterized by the sudden onset of profuse liquid bowel movements and vomiting, leading to severe dehydration and desalination of the body, impaired circulation, cessation of urination, decreased skin temperature, the appearance of convulsions, cyanosis (bluish discoloration of the skin and mucous membranes), profound metabolic disorders and inhibition of central function nervous system up to the development of coma. The probability of death is 60-80%.
Cholera pathogens enter the external environment with feces, and less often with vomit of people.
The main way cholera spreads is through the consumption of contaminated water and contaminated food, and failure to observe personal hygiene rules. Flies also contribute to the spread of infection.
Treatment: Often the disease is asymptomatic or with weak liquid stools, requiring virtually no treatment. In more severe cases, treatment is aimed at restoring the water-salt balance, i.e. the patient is given a large amount of water-salt mixtures and glucose in various ways: through the mouth, using a gastric tube and intravenously. In addition, antibiotics are used for treatment.
Anthrax- a disease from the group of especially dangerous infections that affects farm animals and humans.
The causative agent, anthrax bacillus, has vegetative and spore forms. The vegetative form is resistant to unfavorable environmental conditions, but quickly dies when heated (instantly when boiled) and under the influence of disinfectants. Spores formed outside the body are extremely resistant to any influence; they remain viable and virulent for decades.
The source of infection are domestic herbivores: sheep, goats, cows. Cases of infection from sick people have not been described. Anthrax bacillus is excreted in the urine, feces and saliva of animals. Human infection is possible through contact with sick animals, with contaminated soil, during the processing of anthrax animal raw materials, through finished products made of leather, fur, food and air. There are known cases of laboratory infection with anthrax, as well as infection through receipt of contaminated correspondence. Agricultural workers, farmers, and veterinarians are at increased risk of infection; cases of the disease among travelers and tourists are possible.
The disease is recorded in zoonotic foci* of anthrax in all climatic zones. Sporadic cases or outbreaks are possible. Anthrax in humans can occur in the skin, pulmonary and intestinal forms. The incubation period usually lasts from 2 to 5 days.
Onset of the disease pulmonary form resembles ARVI, but after 3-5 days acute infection develops respiratory failure, which leads to shock and death of the patient.
At cutaneous form The disease first appears as itchy skin and a rash at the entrance gate of the infection. After 2-6 days, the rash turns into blisters, then the tissues die, a black scab is formed, surrounded by edema and secondary small blisters. Sepsis (general blood poisoning) is possible.
During development intestinal form Characterized by cutting pain in the abdomen, vomiting of bile mixed with blood, significant bloating
intestines, frequent loose stool with an admixture of blood, severe intoxication of the body is expressed, and the development of “acute abdomen” syndrome is possible.
The probability of death is 100%. The method of anthrax vaccination was first proposed by the French microbiologist Louis Pasteur.
Control measures: prescribing antibiotics, disinfection, immunization of persons at occupational risk of infection, as well as timely destruction of the corpses of dead sick animals (they are burned or buried deep after treatment with quicklime).
Human anthrax disease is observed in almost all countries of the world. In the past, anthrax was one of the most common infectious diseases. Currently, this disease is common in economically backward, agricultural countries. IN developed countries The disease occurs in isolated cases, mainly associated with the processing of imported raw materials of animal origin. Recently, international attention has been paid to anthrax caused by a number of terrorist attacks that occurred in 2001 in the United States.
Smallpox natural- severe highly contagious human disease. The monuments of ancient writing describe terrible smallpox epidemics that were devastating
smart character. In the XVII-XVIII centuries. In Europe, 10 million people suffered from smallpox every year, about 1.5 million of them died. In the 16th century Spanish colonialists brought the disease to America, where it caused severe epidemics among the Indians. Later it appeared in Australia and Oceania. The world's first smallpox vaccination was made by the English doctor Edward Jenner in 1796.
The incubation period of the disease lasts 12-15 days. Symptoms: chills, high fever, headache, dizziness, vomiting, loss of appetite, constipation; characterized by pain in the lower back and sacrum; possible loss of consciousness, delirium, shortness of breath.
After a slight decrease in temperature, a pinpoint, spotted rash appears throughout the body, especially abundant on the face and hands. Similar rashes cover the mucous membranes oral cavity, nose, conjunctiva of both eyes. As a result, the patient finds it difficult to breathe through the nose, photophobia, lacrimation and salivation develop, and hoarseness and cough appear. The rash very quickly transforms into compactions, then into blisters and pustules, which dry out and form crusts. Following this, itching of the skin and mucous membranes appears. Patients, unable to withstand the itching, tear off the crusts, under which bleeding and suppurating ulcers form. After the crusts are rejected, reddish spots remain, which over time acquire a brown tint, and in those places where the skin lesions were the deepest, round scars (pockmarks) are formed that last a lifetime. As a result of damage to the conjunctiva, blindness can occur. This is the typical clinical picture of smallpox. However, the disease can occur in different ways. The probability of death is 95-100%.
There is no specific treatment for smallpox yet. Prescription of antibiotics prevents the development purulent processes possible when the disease is complicated by a secondary infection.
In 1980, at the XXXIII session of the World Health Assembly, the elimination of this dangerous infection on Earth was announced. However, due to the existence of so-called “monkeypox”, which in an unimmunized population can lead to an outbreak of smallpox in humans, the problem cannot be completely closed.
Viral hepatitis. Hepatitis is an acute infectious disease primarily affecting the liver. To date, five etiological forms of hepatitis have been studied: A, B, C, D (delta hepatitis), E. The incidence of hepatitis remains quite high everywhere. In case of sharp deterioration, sanitary to unfavorable environmental conditions. The source of infection is a sick person; he is contagious from the end of the incubation period. The incubation period lasts, as a rule, 28-30 days. Hepatitis A is also called jaundice or Botkin's disease.
The mechanism of transmission of infection is water-food. People are highly susceptible to this virus, especially in children aged 2 to 10 years.
Symptoms of the disease: sudden onset of illness, fever, general weakness. The patient is worried about lack of appetite, nausea, and abdominal pain. After about a week, jaundice develops, urine becomes dark and feces become discolored, liver function is impaired, and the liver increases in size.
Viral hepatitis B(whey). The causative agent is the hepatitis B virus (HBV), which is quite resistant in the external environment. The source of infection is a sick person. Infection occurs when the virus enters the blood directly through injection or through mucous membranes or damaged skin.
The onset of the disease is gradual, decreased appetite, normal or slightly elevated temperature, abdominal pain, nausea, and sometimes joint pain. After a few days, as with hepatitis A, jaundice develops. The disease can develop into chronic hepatitis, liver cirrhosis, liver cancer, necrosis (death) of the liver, fulminant course of the disease, and coma are possible.
Viral hepatitis D(delta hepatitis). According to the epidemiological features, hepatitis D is similar to hepatitis B, but it is milder. The only source of pathogens is a sick person or a virus carrier. The disease is transmitted through infected blood during transfusion, through direct contact with a patient or virus carrier, or through transfusion of whole blood substitutes.
Hepatitis D is common, like other forms of hepatitis. Complications: in approximately 50% of cases, the disease becomes chronic, and liver cirrhosis is possible.
Treatment viral hepatitis is carried out only in a hospital. There is no specific therapy; treatment measures consist of following a regimen, diet, and prescribing symptomatic medications. Bed rest is mandatory in all cases of viral hepatitis, since restriction of movements reduces energy costs and slows down metabolism. Semi-bed rest is allowed only if the condition improves. general condition patient at the end of the icteric period with very mild forms of the disease.
Tick-borne encephalitis - acute infectious disease of the brain. The causative agent is a filterable virus. The carriers of the virus in nature are pasture and forest ticks. Carriers of the virus: chipmunks, mouse-like rodents, moles, hedgehogs, some species of birds (bunkings, hazel grouse, blackbirds, nuthatches, etc.).
The virus enters the human blood through the saliva of an infected tick during a bite. The incubation period lasts 10-14 days. Tick-borne encephalitis, caused by the activity of ticks, has a pronounced seasonal character - from early spring (the first bites may appear as early as the first warm days of April) until mid-summer, and sometimes until late autumn, until the end of November.
Most often, the disease begins suddenly: a severe headache appears, body temperature rises to 39-40 ° C, nausea, vomiting, general stupor, convulsions, and unconsciousness occur. Paralysis of the limbs may develop. After recovery, strong and long-lasting immunity is developed. On for a long time The patient continues to have headaches and symptoms of nervous system weakness.
Primary means treatment tick-borne encephalitis - anti-encephalitis gamma globulin, preferably human, with high content(titer) of antibodies. In addition, oxygen, restorative and symptomatic therapy, and spinal puncture are used. Antibiotics and sulfonamides, which do not have an antiviral effect, are used only in the event of a secondary infection. If necessary, intensive care and resuscitation are also provided.
Tularemia- acute infectious natural focal disease of humans and animals. The causative agent is a bacterium that is resistant to unfavorable environmental factors, which retains its properties for a long time at low temperatures, but dies instantly when boiled.
Under natural conditions, the sources of infection are rodents and hares. The pathogen is transmitted by ixodid ticks, mosquitoes, and fleas.
A person becomes infected with tularemia as a result of:
direct contact with rodents (voles, water rats, muskrats,
hamsters, etc.);
· “contact with blood or tissues of infected wild animals;
arthropod bites;
Eating animal meat that has not been subjected to prolonged heat
howl processing;
consumption of infected drinking water;
· inhalation of mixed dust.
Tularemia is not transmitted from person to person. Depending on the conditions of infection and the method of transmission of the pathogen, vector-borne, waterborne, commercial, agricultural, household, food and hunting types of epidemic foci of tularemia are distinguished.
The incubation period lasts from 2 to 10 days, but usually 3 days. Symptoms and course of the disease: sudden onset, chills, enlarged and painful lymph nodes, their suppuration, sweating, headache, muscle pain, enlarged liver and spleen. Pulmonary and intestinal, as well as generalized forms of the disease are possible.
Treatment: antibiotics, symptomatic therapy, administration of killed vaccine.
Typhus- an acute infectious disease caused by Provacek's rickettsia. The source of infection is a sick person, the transmitter is a body louse. Infection occurs when excrement from crushed lice gets into the bite site or when dust containing excrement from infected lice is inhaled.
The disease is recorded in endemic foci in regions with cool climates in lice-infested population groups. As a rule, outbreaks occur in overcrowded housing among refugees, as well as among disaster victims.
After a 1-2 week incubation period, the patient suddenly develops a fever, chills, headache, generalized pain, a state of complete physical and neuropsychic relaxation (prostration), and possible delirium. After 5-6 days, a rash appears on the skin of the trunk and limbs (except for the face, palms and soles), which later takes on the character of pinpoint hemorrhages. Complications: acute vascular failure, gangrene, renal failure, coma. After many years, relapses of the disease are possible. The probability of death is 40%.
Treatment: chloramphenicol, tetracycline antibiotics, as well as supportive and symptomatic therapy.
Typhus is common on all continents except Australia. In Russia, the disease appeared about 800 years ago and has always accompanied national disasters - famine, wars, etc. For example, in 1918-1922. In our country, 20 million people have been ill with typhus Typhoid fever - an acute infectious disease that affects only humans. The causative agent of the disease is the typhoid bacillus, which is moderately resistant to adverse environmental conditions, but dies instantly when boiled.
The source of infection is a sick person who sheds bacilli or carries bacteria. The pathogen is transmitted through fecally contaminated food and water. The average incubation period is 14 days.
The disease usually begins gradually. The temperature rises slowly, remains high for 2-3 weeks, then slowly decreases. The patient is worried about nosebleeds, headache, lack of appetite, abdominal pain, and loose stools. Pink spots appear on the skin of the body. Possible states of severe depression, complete immobility, delirium with visual hallucinations. Complications: intestinal bleeding, perforation (breakthrough) of the intestine, pneumonia.
Treatment: antibiotics, blood transfusions, intravenous administration of nutritional mixtures.
Typhoid fever in the 19th - early 20th centuries. was one of the most common and severe infectious diseases in all countries of the world, especially in cities, due to their rapid growth, crowded population and low sanitary and hygienic level. Almost every natural disaster (crop failure, famine, earthquakes), as well as wars, was accompanied by epidemics of typhoid fever.
When you hear that an athlete has dropped dead on the field, this is often the reason. About one in 500 people have some form of hypertrophic cardiomyopathy, which causes the walls of the heart to become thinner, preventing it from doing its job effectively. About 1% of patients die every year, many of them are young and do not even know that they are sick.
What to do Most cases of hypertrophic cardiomyopathy are genetically determined. So ask your parents if there have been cases in the family sudden death at a young age and what was the reason. Many accidents - drowning, car accidents, falls from a horse or motorcycle - can occur due to sudden heart attack in people with undiagnosed cardiomyopathy. If there have been such cases, it is better to ask your doctor to prescribe you an electrocardiogram and ultrasound. You should also look out for unusual symptoms, such as shortness of breath, fainting, and strange heartbeats.
People with this diagnosis can avoid sudden death by being seen by a cardiologist. There are drug and invasive treatments. Any physical activity should be discussed with your doctor.
Electrocardiographic problems
Problems in the system that controls and synchronizes the heart's rate, caused by Brugada syndrome, long QT syndrome, or Wolfe-Parkinson-White syndrome. You may be unaware of anything, and suddenly you have ventricular tachycardia and drop dead.
What to do The causes are also genetic, so talk to your doctor about your family tree. An electrocardiogram and a stress test help identify the problem. Those who have received a diagnosis are observed by a cardiologist and receive drug treatment, pacemakers. The risk of sudden death can be reduced in a healthy way life. Don't smoke and limit yourself to alcohol. And be sure to tell your doctor if you have nightmares: this could be a symptom of Brugada syndrome, which often kills people in their sleep.
Cerebral aneurysm
We are talking about protrusion of the vessel wall due to its thinning or stretching. In most cases, the disease does not warn about itself. However, about a third of these vessels rupture, leading to instant death in 40% of cases.
What to do Sudden, severe headaches should not be ignored, especially if they are accompanied by strange symptoms such as drooping eyelids, double vision before the eyes, or narrowing of one pupil (signs of aneurysm pressure on nerves in the brain).
Early detection often allows surgical removal aneurysm or prescribe medication. Be especially vigilant if you have high blood pressure: This increases the risk of rupture of the damaged vessel.
Aortic dissection
The reasons are still unknown. According to statistics, it occurs in about two out of 10,000 people, most of them men between 40 and 70 years old.
What to do Sudden, excruciating pain in the chest or upper back is the main symptom, so see a doctor immediately if this happens to you. The risk of disease is higher if there is a family history of such cases or if you have a disease connective tissue, such as Ehlers-Danlos syndrome. A recent study suggested that visits for aortic dissection peak during flu season, so consider getting vaccinated.
Pulmonary embolism
A blood clot is not easy to spot. In half of the cases there are no symptoms at all - except for sudden death, which occurs in every fourth case. In the other half, the symptoms are not obvious. Let's say there would be pain and swelling in one arm or leg that doesn't go away within 1-2 days (especially after a long period of inactivity, say after a fracture).
What to do Pay attention to symptoms of blood clots in other places, such as the legs and arms. Using anticoagulants can prevent a blood clot from traveling to the lungs.
It is extremely unpleasant to bring back from a long-awaited vacation a disease that is dangerous not only to health, but also to life. Therefore, when planning a trip, it is worth asking in advance what diseases are common where you are going.
Rospotrebnadzor specialists have compiled a list of common and dangerous diseases, countries where they are common, and measures that will help avoid them.
Diseases:
Route of infection:
Foods (especially raw), swimming in bodies of water.
Incubation period:
Individual prevention:
Compliance with sanitary and hygienic measures: water disinfection, hand washing, heat treatment of food, disinfection of common areas.

Route of infection:
Mosquitoes of the genus "Egyptian".
Incubation period:
From 3 to 6 days.
Individual prevention:
Immunization and use of personal protective equipment against mosquitoes.
Route of infection:
Through direct contact with the blood, secretions, other fluids and organs of an infected person.
Incubation period:
From 2 to 21 days.
Individual prevention:
Specific prevention not developed.
Route of infection:
Incubation period:
From 3 to 17 days.
Individual prevention:
Protecting your home from rats.
Route of infection:
Animals, rodents, sick people.
Incubation period:
From 3 to 17 days.
Individual prevention:
Barrier protection of household items and products from contamination by rodent urine or dust containing their excrement.
Route of infection:
Malaria mosquito bite.
Incubation period:
From 7 days to 1 month.
Individual prevention:
Taking antimalarial drugs.
Route of infection:
When bitten by infected fleas, sick animals and rodents, by airborne droplets when communicating with a patient with pneumonic plague.
Incubation period:
From several hours to 6 days.
Individual prevention:
Strict adherence to sanitary and hygienic rules.
Route of infection:
In case of contact with infected, dead poultry or wild poultry, consumption of meat and eggs of sick birds without sufficient heat treatment.
Incubation period:
From several hours to 5 days.
Individual prevention:
Flu vaccination at least 2 weeks before travel.
Cholera
Cholera is a very dangerous acute infectious disease, characterized by severe dehydration of the body, which in the absence of timely treatment can lead to death.
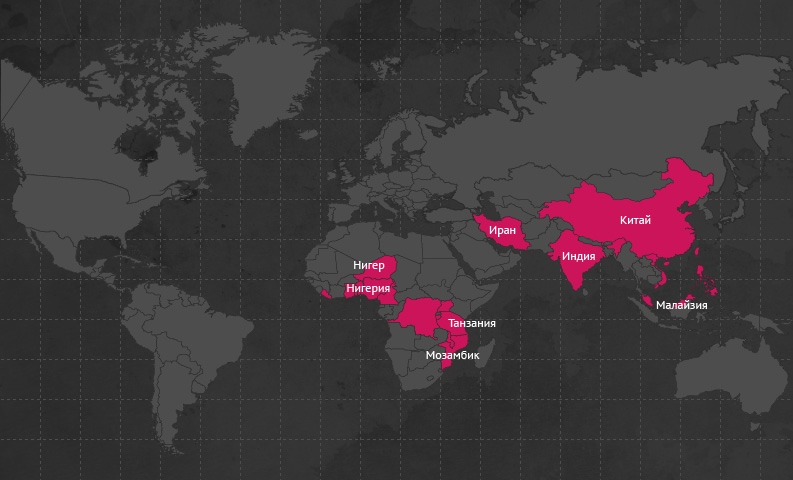
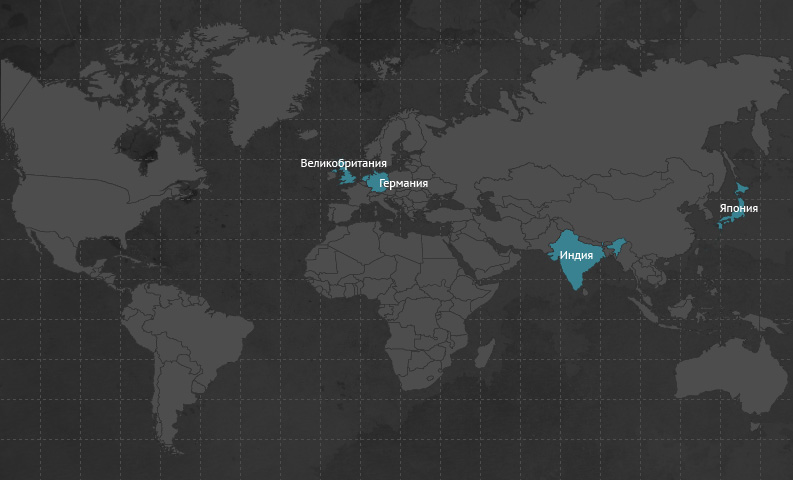
Cases of cholera are registered annually in the countries of Asia and Southeast Asia: in India, Iran, China, Malaysia, Vietnam, Singapore and the Philippines, and imported cases of cholera are registered in Europe, the USA, Australia and Oceania.
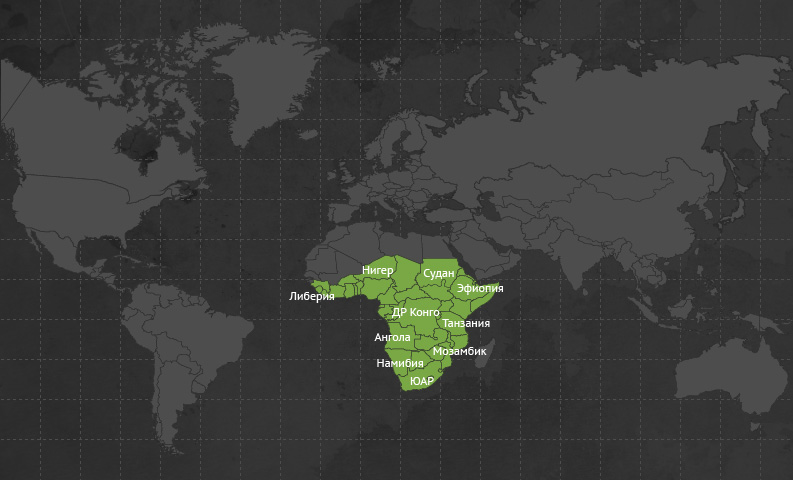
In Africa, cholera patients are registered annually in Benin, Burundi, Ghana, the Democratic Republic of the Congo, Cameroon, Liberia, Malawi, Mozambique, Niger, Nigeria, Tanzania, Togo, and Uganda.
The incubation period (hidden or latent period of the disease) is the period of time from the moment the microbial agent enters the body until the symptoms of the disease appear. That is, the person is already infected, but the disease has not yet manifested itself. The duration of the incubation period can vary from several hours and even minutes to tens of years. As a rule, during the incubation period, a sick person is not contagious to others, but with some diseases, the release of microbes through saliva, coughing and sneezing begins 1-3 days before the onset of the disease. Often, during the incubation period, it is already possible to detect the pathogen itself or antibodies to it in the body and begin treatment.
Path of infection. Cholera pathogens enter the human body through consumption of contaminated food and water, and the most dangerous are foods that are not heat-treated. Infection can also occur while swimming in water bodies.
- from several hours to 5 days.
Characteristic signs- repeated loose stools and vomiting, which leads to dehydration.
What to do? When the first signs of the disease appear, you should immediately consult a doctor.
Yellow fever
Yellow fever is common in 32 African countries and 12 countries South America(Angola, Benin, Burkina Faso, Burundi, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Democratic Republic of the Congo, Cameroon, Kenya, Congo, Ivory Coast, Liberia, Mauritania, Mali, Niger, Nigeria, Rwanda , Sao Tome and Principe, Senegal, Somalia, Sudan, Sierra Leone, Tanzania, Togo, Uganda, Central African Republic, Chad, Equatorial Guinea and Ethiopia, Bolivia, Brazil, Venezuela, Guyana, French Guiana, Colombia, Panama, Peru, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago, Ecuador).
Path of infection. Yellow fever is transmitted by mosquitoes of the “Egyptian” genus; you can become infected both in natural conditions and in cities.Incubation period of the disease- from 3 to 6 days.
Characteristic signs. The disease is characterized high fever, hemorrhagic rash, kidney damage, liver with the development of jaundice and acute renal failure. The course of the disease is extremely severe and in most cases is fatal.
What to do? Protect yourself from the disease in advance. Thus, when traveling to the countries of the South American and African continents, where mandatory preventive vaccinations, which is the only measure to prevent this dangerous disease, it is necessary to receive a single vaccination, which is carried out no later than 10 days before departure, immunity remains for 10 years, after which a second vaccination is carried out. Without an international certificate of vaccination against yellow fever, travel to disadvantaged countries is prohibited.
Ebola, Marburg and Lassa
These fevers are considered severe viral diseases with almost the same clinical picture. In particular, fevers are manifested by high fever, hemorrhagic rash, bleeding from the nose, gums, blood in the stool and vomit, headaches, general weakness, pain in the chest and stomach.
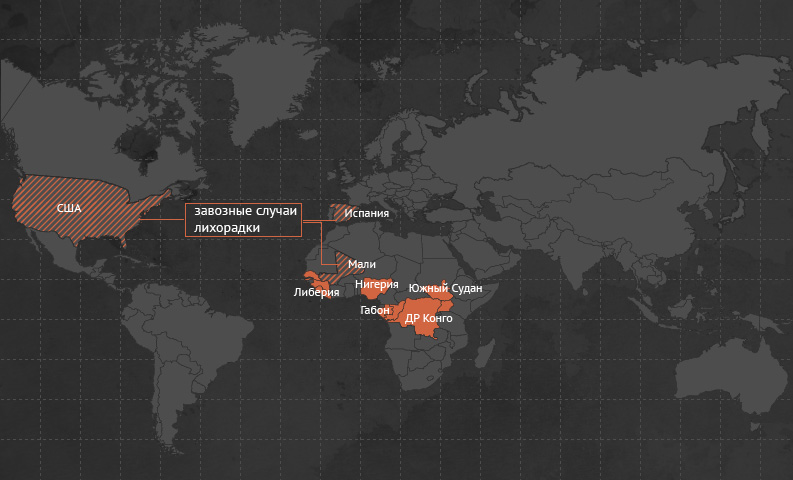
Ebola fever has been reported in Uganda, Gabon and the Republic of Congo, South Sudan, and the Democratic Republic of Congo.Path of infection: through direct contact with blood, secretions, other fluids and organs of an infected person.
Incubation period- from 2 to 21 days.
What to do? Specific prevention against this disease has not been developed.
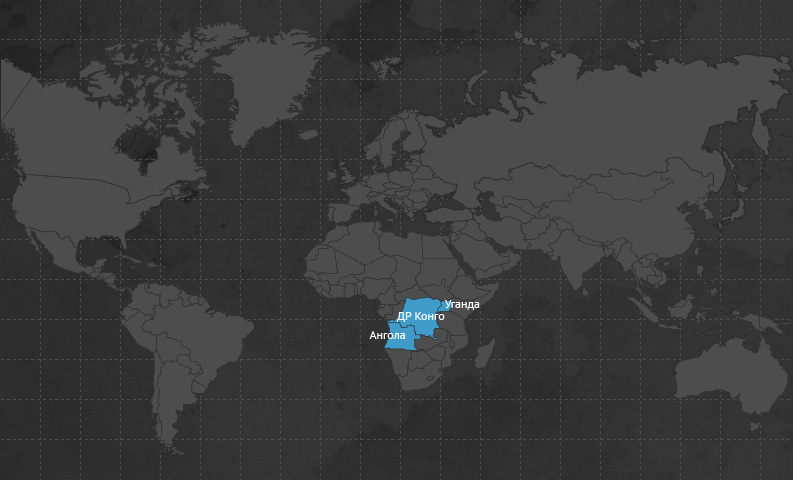
Marburg hemorrhagic fever registered in the Democratic Republic of the Congo, Angola, Uganda.
Path of infection
Incubation period- from 3 to 17 days.
What to do? Protect your place of residence from rats.
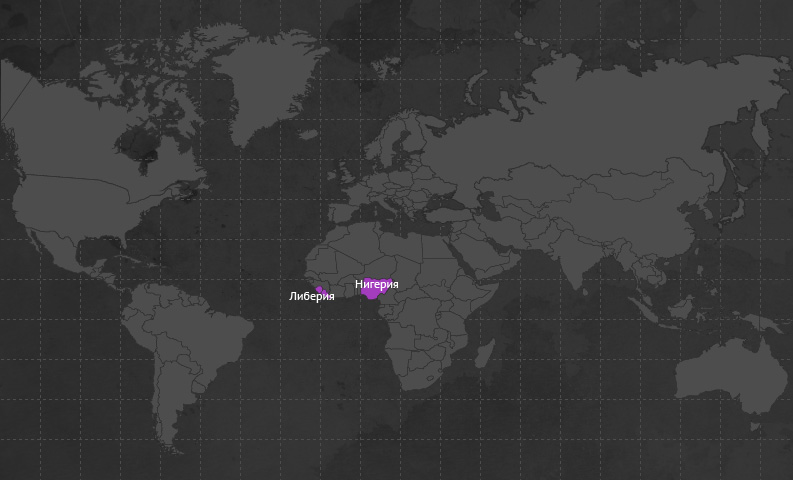
Lassa fever registered in Sierra Leone, Nigeria, Liberia.
Path of infection: animals, rodents, sick person.
Incubation period- from 3 to 17 days.
What to do? Use barrier methods to protect household items and products from contamination by rodent urine or dust containing rodent excrement.
Malaria
Path of infection: for bites of malaria mosquitoes.Incubation period. From 7 days to 1 month for tropical malaria and up to 3 years for other forms.
Characteristic signs. Symptoms of the disease are fever, chills, heavy sweating, headache, weakness.
What to do? For the purpose of prevention, it is necessary to regularly take antimalarial drugs. Taking medications should begin 1 week before leaving abroad, continue throughout the entire period of stay and 1 month after returning.
At the first symptoms and the slightest suspicion of the disease, it is important to seek medical help as quickly as possible, since with tropical malaria, without timely treatment, death is possible in a very short time from the onset of the disease.
Pneumonic plague
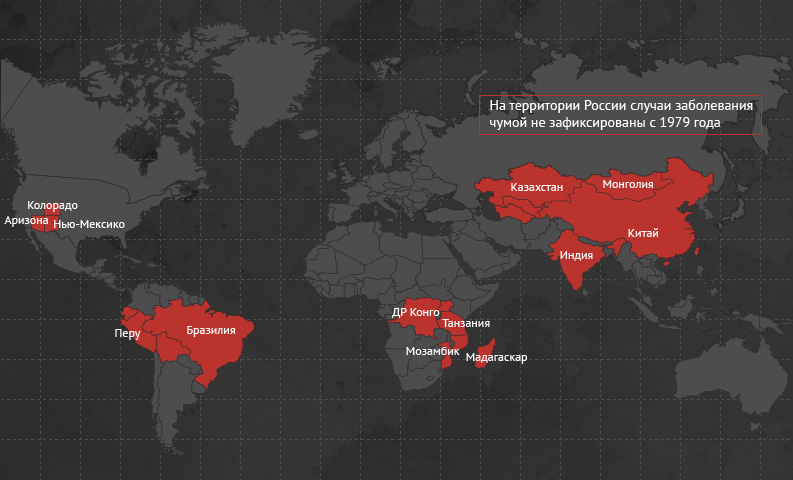
Plague is widespread in the Democratic Republic of the Congo, India, Madagascar, Mozambique, Uganda and Tanzania, as well as in Central Asia, such as Kazakhstan, Turkmenistan, Uzbekistan and Mongolia. In China, there are outbreaks of plague in 19 provinces. On the American continent, permanent natural foci of plague exist in Brazil, Bolivia, Peru, Ecuador and the United States of America.
Path of infection. Infection with plague occurs through bites by infected fleas, contact with sick animals and rodents, as well as through airborne droplets when communicating with a patient with pneumonic plague.
Incubation period. The time that passes from the moment the plague pathogen enters the human body until the first symptoms of the disease appear ranges from several hours to 6 days.
Characteristic signs. The disease begins with high temperature, severe chills, headache, swollen lymph nodes and coughing up blood.
What to do? If these signs of the disease appear, you should immediately consult a doctor.
Bird flu
Avian influenza is an acute infectious disease caused by a virus.
Path of infection. Human infection occurs through close contact with infected live or dead poultry and wild birds. Sometimes it is possible for humans to become infected by eating meat and eggs of sick birds without sufficient heat treatment. Also dangerous are the secretions of infected birds, which, when they fall on plants, into the air, into water, can then infect humans through water when drinking and bathing, as well as through airborne droplets, airborne dust and through dirty hands.
Incubation period- from several hours to 5 days.Characteristic signs. The disease with avian influenza begins acutely, with unexpected chills, fever up to 38°C and above, muscle pain, headaches, and sore throat. Possible watery, loose stools and repeated vomiting. The patient's condition usually deteriorates quickly. After 2-3 days it appears wet cough, often mixed with blood, shortness of breath. Difficulty breathing may occur, and damage to the liver, kidneys and brain may also occur.
What to do? When the first signs of the disease appear, you must immediately consult a doctor to establish a diagnosis and prescribe adequate and timely treatment. Late initiation of treatment inevitably leads to the development of complications.
Prevention measures. It is necessary to avoid contact with poultry and wild birds in households, markets and places where birds gather in large numbers on open water bodies.
Intimate infections
During casual sex, everyone runs the risk of becoming infected dangerous infections, including AIDS, syphilis, viral hepatitis IN.
For warning specified diseases always carry and use personal protective equipment and avoid questionable sexual contacts.
HIV infection
HIV is a chronic, slow viral infection.
Incubation period. The latent period of HIV infection ranges from several months to several years.
Path of infection. The infection is mainly transmitted sexually, through the use of blood-contaminated medical instruments and syringes when injecting drugs, through donor organs and tissues from patients with HIV infection. Remembering the possibility of contracting this infection is extremely important if you plan to travel to countries where a system for monitoring donor blood has not yet been established and there is a danger of using non-sterile medical equipment when providing medical care, especially in dentistry.
Having become infected with HIV, a person becomes a virus carrier and, while remaining practically healthy for a long time, can infect his sexual partners.
The final stage of HIV infection is AIDS - acquired human immunodeficiency syndrome, in which progressive destruction occurs immune system a person that cannot be treated and ends in death within a year.
What to do? To prevent HIV infection, you must independently take care of a supply of disposable syringes and condoms, and before going on vacation, visit the dentist.
